Are Fallen Arches Flat Feet?
Overview
_(B)_Adult_foot_that_has_never_worn_shoes,_(Right)_(A)_Foot_of_a_boy_who_has_worn_shoes_for_just_a_few_weeks._Plaster_casts.jpg)
A variety of foot problems can lead to adult acquired flatfoot deformity (AAFD), a condition that results in a fallen arch with the foot pointed outward. Most people - no matter what the cause of their flatfoot - can be helped with orthotics and braces. In patients who have tried orthotics and braces without any relief, surgery can be a very effective way to help with the pain and deformity. This article provides a brief overview of the problems that can result in AAFD. Further details regarding the most common conditions that cause an acquired flatfoot and their treatment options are provided in separate articles. Links to those articles are provided.
Causes
Most cases of flatfeet are simply the result of normal development. When that is not the case, the condition can be caused by a number of factors, including the following, Age, disease, injury, obesity or being overweight, physical abnormality, pregnancy. Flattened arches in adults may result from the stresses of aging, weight gain, and the temporary increase in elastin (protein in connective tissue) due to pregnancy. In some cases, flatfeet are caused by a physical abnormality, such as tarsal coalition (two or more bones in the foot that have grown together) or accessory navicular (an extra bone along the side of the foot). The effects of diseases such as diabetes and rheumatoid arthritis can lead to flatfeet. An injury (e.g., bone fracture, dislocation, sprain or tear in any of the tendons and ligaments in the foot and leg) also can cause flatfeet.
Symptoms
Having flat feet can be painless and is actually normal in some people. But others with flat feet experience pain in the heel or arch area, difficulty standing on tiptoe, or have swelling along the inside of the ankle. They may also experience pain after standing for long periods of time or playing sports. Some back problems can also be attributed to flat feet.
Diagnosis
You can test yourself to see if you have flat feet or fallen arches by using a simple home experiment. First, dip your feet in water. Then step on a hard flat surface, like a dry floor or a piece of paper on the floor, where your footprints will show. Step away and examine your foot prints. If you see complete/full imprints of your feet on the floor, you may have fallen arches. However, it?s important to seek a second option from a podiatrist if you suspect you have fallen arches so they can properly diagnose and treat you.
Non Surgical Treatment
The treatment your podiatrist recommends will depend upon the trouble and pain you?re experiencing. Custom shoe inserts (orthotics) are most often recommended and are quite effective. Stretching exercises to loosen and strengthen the supporting tendons may also be recommended. Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may recommend an ankle brace or a custom orthotic device that fits into your shoe to support the arch. A short-leg cast or boot may be worn to immobilize the foot and allow the tendon to heal. Ultrasound therapy and stretching exercises may help rehabilitate the tendon and muscle following immobilization. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Your foot and ankle surgeon may recommend changes in your footwear.
Surgical Treatment

Generally one of the following procedures is used to surgically repair a flat foot or fallen arch. Arthrodesis. One or more of your bones in the foot or ankle are fused together. Osteotomy. Correcting alignment by cutting and reshaping a bone. Excision. Removing a bone or a bone spur. Synovectomy. Cleaning the sheath that covers the tendon. Tendon transfer. Using a piece of one tendon to lengthen or replace another. Arthroereisis. placing a small device in the subtalar joint to limit motion. For most people, treatment is successful, regardless of the cause, although the cause does does play a major role in determining your prognosis. Some causes do not need treatment, while others require a surgical fix.
Prevention
oll away pain. If you're feeling pain in the arch area, you can get some relief by massaging the bottom of your foot. A regular massage while you're watching TV can do wonders" Stretch out. Doing the same type of stretching exercises that runners do in their warm-up can help reduce arch pain caused by a tight heel cord. One of the best exercises is to stand about three feet from a wall and place your hands on the wall. Leaning toward the wall, bring one foot forward and bend the knee so that the calf muscles of the other leg stretch. Then switch legs. Stretching is particularly important for women who spend all week in heels and then wear exercise shoes or sneakers on weekends. Get measured each time you buy new shoes. Don't assume that since you always wore a particular size, you always will. Too many people try to squeeze into their 'regular' shoe size and wind up with serious foot problems or sores on their feet. When your arch is falling, your feet may get longer or wider and you may or may not feel pain, so getting your foot measured each time you buy shoes is a good indicator of your arch's degeneration. Examine your shoes. If the heel is worn down, replace it. But if the back portion of the shoe is distorted or bent to one side, get yourself into a new pair of supportive shoes like those made specifically for walking. That's because flat feet can affect your walking stride, and failing to replace worn shoes may lead to knee or hip pain.
_(B)_Adult_foot_that_has_never_worn_shoes,_(Right)_(A)_Foot_of_a_boy_who_has_worn_shoes_for_just_a_few_weeks._Plaster_casts.jpg)
A variety of foot problems can lead to adult acquired flatfoot deformity (AAFD), a condition that results in a fallen arch with the foot pointed outward. Most people - no matter what the cause of their flatfoot - can be helped with orthotics and braces. In patients who have tried orthotics and braces without any relief, surgery can be a very effective way to help with the pain and deformity. This article provides a brief overview of the problems that can result in AAFD. Further details regarding the most common conditions that cause an acquired flatfoot and their treatment options are provided in separate articles. Links to those articles are provided.
Causes
Most cases of flatfeet are simply the result of normal development. When that is not the case, the condition can be caused by a number of factors, including the following, Age, disease, injury, obesity or being overweight, physical abnormality, pregnancy. Flattened arches in adults may result from the stresses of aging, weight gain, and the temporary increase in elastin (protein in connective tissue) due to pregnancy. In some cases, flatfeet are caused by a physical abnormality, such as tarsal coalition (two or more bones in the foot that have grown together) or accessory navicular (an extra bone along the side of the foot). The effects of diseases such as diabetes and rheumatoid arthritis can lead to flatfeet. An injury (e.g., bone fracture, dislocation, sprain or tear in any of the tendons and ligaments in the foot and leg) also can cause flatfeet.
Symptoms
Having flat feet can be painless and is actually normal in some people. But others with flat feet experience pain in the heel or arch area, difficulty standing on tiptoe, or have swelling along the inside of the ankle. They may also experience pain after standing for long periods of time or playing sports. Some back problems can also be attributed to flat feet.
Diagnosis
You can test yourself to see if you have flat feet or fallen arches by using a simple home experiment. First, dip your feet in water. Then step on a hard flat surface, like a dry floor or a piece of paper on the floor, where your footprints will show. Step away and examine your foot prints. If you see complete/full imprints of your feet on the floor, you may have fallen arches. However, it?s important to seek a second option from a podiatrist if you suspect you have fallen arches so they can properly diagnose and treat you.
Non Surgical Treatment
The treatment your podiatrist recommends will depend upon the trouble and pain you?re experiencing. Custom shoe inserts (orthotics) are most often recommended and are quite effective. Stretching exercises to loosen and strengthen the supporting tendons may also be recommended. Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may recommend an ankle brace or a custom orthotic device that fits into your shoe to support the arch. A short-leg cast or boot may be worn to immobilize the foot and allow the tendon to heal. Ultrasound therapy and stretching exercises may help rehabilitate the tendon and muscle following immobilization. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Your foot and ankle surgeon may recommend changes in your footwear.
Surgical Treatment

Generally one of the following procedures is used to surgically repair a flat foot or fallen arch. Arthrodesis. One or more of your bones in the foot or ankle are fused together. Osteotomy. Correcting alignment by cutting and reshaping a bone. Excision. Removing a bone or a bone spur. Synovectomy. Cleaning the sheath that covers the tendon. Tendon transfer. Using a piece of one tendon to lengthen or replace another. Arthroereisis. placing a small device in the subtalar joint to limit motion. For most people, treatment is successful, regardless of the cause, although the cause does does play a major role in determining your prognosis. Some causes do not need treatment, while others require a surgical fix.
Prevention
oll away pain. If you're feeling pain in the arch area, you can get some relief by massaging the bottom of your foot. A regular massage while you're watching TV can do wonders" Stretch out. Doing the same type of stretching exercises that runners do in their warm-up can help reduce arch pain caused by a tight heel cord. One of the best exercises is to stand about three feet from a wall and place your hands on the wall. Leaning toward the wall, bring one foot forward and bend the knee so that the calf muscles of the other leg stretch. Then switch legs. Stretching is particularly important for women who spend all week in heels and then wear exercise shoes or sneakers on weekends. Get measured each time you buy new shoes. Don't assume that since you always wore a particular size, you always will. Too many people try to squeeze into their 'regular' shoe size and wind up with serious foot problems or sores on their feet. When your arch is falling, your feet may get longer or wider and you may or may not feel pain, so getting your foot measured each time you buy shoes is a good indicator of your arch's degeneration. Examine your shoes. If the heel is worn down, replace it. But if the back portion of the shoe is distorted or bent to one side, get yourself into a new pair of supportive shoes like those made specifically for walking. That's because flat feet can affect your walking stride, and failing to replace worn shoes may lead to knee or hip pain.
Fallen Arches What To Expect
Overview

Flat feet plague many Americans and perhaps one of the worst times to have fallen arches is the winter holiday season. Why? Many people are destined to spend hours standing in line waiting to pay for holiday gifts, see Santa or mail holiday cards and packages. There are also those cocktail parties, holiday caroling sessions and strolls through the Christmas lights that will undoubtedly have people on their feet for long stretches of time too.
Causes
Flat feet in adults can arise from a variety of causes. Here are the most common. An abnormality that is present from birth, stretched or torn tendons, damage or inflammation of the posterior tibial tendon (PTT), which connects from your lower leg, along your ankle, to the middle of the arch, broken or dislocated bones. Some health conditions, such as rheumatoid arthritis, Nerve problems. Other factors that can increase your risk include obesity, diabetes, ageing and Pregnancy.
Symptoms
Many people have flat feet and notice no problems and require no treatment. But others may experience the following symptoms, Feet tire easily, painful or achy feet, especially in the areas of the arches and heels, the inside bottom of your feet become swollen, foot movement, such as standing on your toes, is difficult, back and leg pain, If you notice any of these symptoms, it's time for a trip to the doctor.
Diagnosis
If your child has flatfeet, his or her doctor will ask about any family history of flatfeet or inherited foot problems. In a person of any age, the doctor will ask about occupational and recreational activities, previous foot trauma or foot surgery and the type of shoes worn. The doctor will examine your shoes to check for signs of excessive wear. Worn shoes often provide valuable clues to gait problems and poor bone alignment. The doctor will ask you to walk barefoot to evaluate the arches of the feet, to check for out-toeing and to look for other signs of poor foot mechanics. The doctor will examine your feet for foot flexibility and range of motion and feel for any tenderness or bony abnormalities. Depending on the results of this physical examination, foot X-rays may be recommended. X-rays are always performed in a young child with rigid flatfeet and in an adult with acquired flatfeet due to trauma.
Non Surgical Treatment
Flat feet and fallen arches can be treated effectively by wearing an orthotic insert in your shoes. Orthotics can be custom-made and prescribed by your foot specialist (podiatrist), or you can use a so called pre-made foot orthotic. Most people do not require expensive custom-made orthotics to combat excess pronation, unless they have a specific medical foot condition. Orthotic insoles were developed to correct excess pronation, thereby providing sustainable, long-lasting pain relief to many aches and pains in a natural way. Comfort, Casual and Sports are products which promote excellent biomechanical control of the foot.
Surgical Treatment

A better approach is to strengthen the weakened ligaments with Prolotherapy, supplemented by an arch support if the condition has existed for several years. Chronic pain is most commonly due to tendon and ligament weakness, or cartilage deterioration. The safest and most effective natural medicine treatment for repairing tendon, ligament and cartilage damage is Prolotherapy. In simple terms, Prolotherapy stimulates the body to repair painful areas. It does so by inducing a mild inflammatory reaction in the weakened ligaments and cartilage. Since the body heals by inflammation, Prolotherapy stimulates healing. Prolotherapy offers the most curative results in treating chronic pain. It effectively eliminates pain because it attacks the source: the fibro-osseous junction, an area rich in sensory nerves. What?s more, the tissue strengthening and pain relief stimulated by Prolotherapy is permanent.
Prevention
Wear Supportive Footwear. Spend the money it takes to get proper fitting and quality footwear with good arch supports. Most sufferers of fallen arches and plantar fasciitis are born with high arches that sag as they get older. Good footwear can prevent this from becoming a problem. Flat feet, however, can become just as problematic. So, really we should all be wearing good footwear to avoid this potentially painful condition. Take It Easy. If your heel starts to hurt, take a rest. If the pain doesn?t go away after several days of resting, it may be time to see a podiatrist. Orthotics. Special insoles to support the arch of the foot can provide some much needed help. You can buy these at your local drugstore (not recommended), or you can have them specially made and custom fit for your feet. It can take awhile to get just the right one for your foot, but sometimes it can be just what you needed. Weight Control. Yes, maintaining a sensible diet with your ideal weight can be beneficial in many ways. It makes sense to think that the more weight your arches are supporting, the more easily they will fall and become painful.

Flat feet plague many Americans and perhaps one of the worst times to have fallen arches is the winter holiday season. Why? Many people are destined to spend hours standing in line waiting to pay for holiday gifts, see Santa or mail holiday cards and packages. There are also those cocktail parties, holiday caroling sessions and strolls through the Christmas lights that will undoubtedly have people on their feet for long stretches of time too.
Causes
Flat feet in adults can arise from a variety of causes. Here are the most common. An abnormality that is present from birth, stretched or torn tendons, damage or inflammation of the posterior tibial tendon (PTT), which connects from your lower leg, along your ankle, to the middle of the arch, broken or dislocated bones. Some health conditions, such as rheumatoid arthritis, Nerve problems. Other factors that can increase your risk include obesity, diabetes, ageing and Pregnancy.
Symptoms
Many people have flat feet and notice no problems and require no treatment. But others may experience the following symptoms, Feet tire easily, painful or achy feet, especially in the areas of the arches and heels, the inside bottom of your feet become swollen, foot movement, such as standing on your toes, is difficult, back and leg pain, If you notice any of these symptoms, it's time for a trip to the doctor.
Diagnosis
If your child has flatfeet, his or her doctor will ask about any family history of flatfeet or inherited foot problems. In a person of any age, the doctor will ask about occupational and recreational activities, previous foot trauma or foot surgery and the type of shoes worn. The doctor will examine your shoes to check for signs of excessive wear. Worn shoes often provide valuable clues to gait problems and poor bone alignment. The doctor will ask you to walk barefoot to evaluate the arches of the feet, to check for out-toeing and to look for other signs of poor foot mechanics. The doctor will examine your feet for foot flexibility and range of motion and feel for any tenderness or bony abnormalities. Depending on the results of this physical examination, foot X-rays may be recommended. X-rays are always performed in a young child with rigid flatfeet and in an adult with acquired flatfeet due to trauma.
Non Surgical Treatment
Flat feet and fallen arches can be treated effectively by wearing an orthotic insert in your shoes. Orthotics can be custom-made and prescribed by your foot specialist (podiatrist), or you can use a so called pre-made foot orthotic. Most people do not require expensive custom-made orthotics to combat excess pronation, unless they have a specific medical foot condition. Orthotic insoles were developed to correct excess pronation, thereby providing sustainable, long-lasting pain relief to many aches and pains in a natural way. Comfort, Casual and Sports are products which promote excellent biomechanical control of the foot.
Surgical Treatment

A better approach is to strengthen the weakened ligaments with Prolotherapy, supplemented by an arch support if the condition has existed for several years. Chronic pain is most commonly due to tendon and ligament weakness, or cartilage deterioration. The safest and most effective natural medicine treatment for repairing tendon, ligament and cartilage damage is Prolotherapy. In simple terms, Prolotherapy stimulates the body to repair painful areas. It does so by inducing a mild inflammatory reaction in the weakened ligaments and cartilage. Since the body heals by inflammation, Prolotherapy stimulates healing. Prolotherapy offers the most curative results in treating chronic pain. It effectively eliminates pain because it attacks the source: the fibro-osseous junction, an area rich in sensory nerves. What?s more, the tissue strengthening and pain relief stimulated by Prolotherapy is permanent.
Prevention
Wear Supportive Footwear. Spend the money it takes to get proper fitting and quality footwear with good arch supports. Most sufferers of fallen arches and plantar fasciitis are born with high arches that sag as they get older. Good footwear can prevent this from becoming a problem. Flat feet, however, can become just as problematic. So, really we should all be wearing good footwear to avoid this potentially painful condition. Take It Easy. If your heel starts to hurt, take a rest. If the pain doesn?t go away after several days of resting, it may be time to see a podiatrist. Orthotics. Special insoles to support the arch of the foot can provide some much needed help. You can buy these at your local drugstore (not recommended), or you can have them specially made and custom fit for your feet. It can take awhile to get just the right one for your foot, but sometimes it can be just what you needed. Weight Control. Yes, maintaining a sensible diet with your ideal weight can be beneficial in many ways. It makes sense to think that the more weight your arches are supporting, the more easily they will fall and become painful.
Achilles Tendon Pain In The Heel
Overview
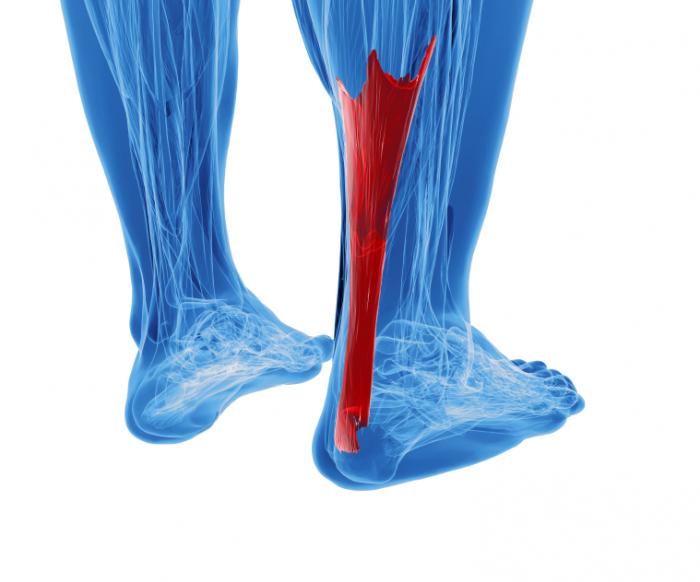 The Achilles tendon connects the calf muscles in the lower leg to the heel bone. It is the largest yet most exposed tendon in the body. Achilles tendonitis is where the Achilles tendon, and sometimes the protective sheath through which it moves, becomes inflamed, causing pain and swelling symptoms. Achilles tendonitis (also known as Achilles tendinopathy or tendonosis) is classified as an overuse injury. If left untreated it can become chronic (long-term), requiring more intensive treatment. Achilles tendonitis can also increase the risk of sustaining an Achilles tendon rupture (tear).
The Achilles tendon connects the calf muscles in the lower leg to the heel bone. It is the largest yet most exposed tendon in the body. Achilles tendonitis is where the Achilles tendon, and sometimes the protective sheath through which it moves, becomes inflamed, causing pain and swelling symptoms. Achilles tendonitis (also known as Achilles tendinopathy or tendonosis) is classified as an overuse injury. If left untreated it can become chronic (long-term), requiring more intensive treatment. Achilles tendonitis can also increase the risk of sustaining an Achilles tendon rupture (tear).
Causes
Short of a trauma, the primary cause of Achilles tendonitis is when the calf muscle is so tight that the heel is unable to come down to the ground placing extreme stress on the Achilles tendon at the insertion. Keep in mind that the calf muscle is designed to contract up, lifting the heel bone off the ground, propelling you forwards to the front of the foot for push off. When the calf is so tight that the heel is prevented from coming down on the ground there will be stress on the tendon and the foot will over pronate causing the Achilles tendon to twist, adding to the stress on the insertion. Improper treatment may lead to a more severe injury, such as a rupture or chronic weakening, which may require surgery.
Symptoms
Symptoms vary because you can injure various areas of the muscle-tendon complex. The pain may be an acute or chronic sharp, stabbing, piercing, shooting, burning or aching. It is often most noticeable immediately after getting out of bed in the morning, or after periods of inactivity, like sitting down for lunch. After a couple minutes of walking around, it will often then settle down somewhat, before becoming symptomatic again after excessive time standing or walking. But regardless of how the pain is perceived, Achilles tendon pain should not be left untreated due to the danger that the tendon can become weak, frayed, thickened, and eventually it may rupture.
Diagnosis
A doctor or professional therapist will confirm a diagnosis, identify and correct possible causes, apply treatment and prescribe eccentric rehabilitation exercises. An MRI or Ultrasound scan can determine the extent of the injury and indicate a precise diagnosis. Gait analysis along with a physical assessment will identify any possible biomechanical factors such as over pronation which may have contributed to the achilles tendonitis and training methods will be considered. Biomechanical problems can be corrected with the use of orthotic inserts and selection of correct footwear.
Nonsurgical Treatment
Massage therapy improves blood flow to the muscles and tissues of the affected area while increasing range of motion and can prevent recurring injury. The healing process can be quickened using ultrasound heat therapy to improve blood flow to the affected area. Wearing a night brace keeps the leg flexed, preventing stiffening of the tendon, which would impair healing. Stretching exercises increase flexibility and allow the tendon to heal without shortening, a deformity resulting in chronic pain. Persistent Achilles pain may warrant the use of a cast or walking boot to be worn for 4-6 weeks stabilizing the tendon so it can heal. After removal of the cast or boot, physical therapy will be ordered to increase functionality of the affected limb. To reduce chronic inflammation of the tendon, corticosteroid injections may be prescribed. It?s important to note that this corticosteroid treatment increases the risk of tendon rupture. Ultrasound imaging may be used by the physician administering the steroid injection, in order to help visualize the affected area. When all other therapies have failed to or tendon rupture occurs, surgical intervention and repair of the muscles and tendons is the last treatment option.

Surgical Treatment
If non-surgical approaches fail to restore the tendon to its normal condition, surgery may be necessary. The foot and ankle surgeon will select the best procedure to repair the tendon, based upon the extent of the injury, the patient?s age and activity level, and other factors.
Prevention
As with all injuries, prevention is your best defense especially with injuries that are as painful and inconvenient as Achilles tendonitis. Options for how to prevent Achilles tendonitis include, stretching- Stretching properly, starting slowly, and increasing gradually will be critical if you want to avoid Achilles tendonitis. To help maintain flexibility in the ankle joint, begin each day with a series of stretches and be certain to stretch prior to, and after, any exercise or excessive physical activity. Orthotics and Heel Support- Bio-mechanically engineered inserts and heel cups can be placed in your shoes to correct misalignments or bolster the support of your foot and are available without a prescription. The temporary heel padding that these provide reduces the length that the Achilles tendon stretches each time you step, making it more comfortable to go about your daily routine. Proper Footwear- Low-heeled shoes with good arch support and shock absorption are best for the health of your foot. Look into heel wedges and other shoe inserts to make sure that your everyday foot mechanics are operating under ideal conditions.
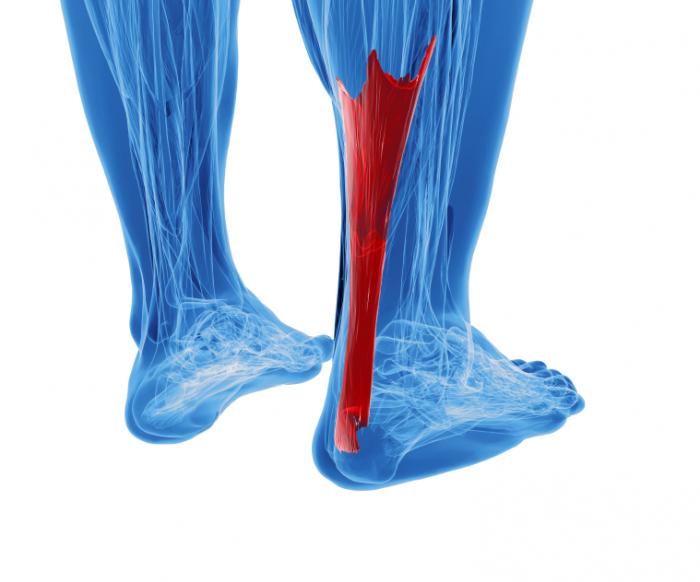 The Achilles tendon connects the calf muscles in the lower leg to the heel bone. It is the largest yet most exposed tendon in the body. Achilles tendonitis is where the Achilles tendon, and sometimes the protective sheath through which it moves, becomes inflamed, causing pain and swelling symptoms. Achilles tendonitis (also known as Achilles tendinopathy or tendonosis) is classified as an overuse injury. If left untreated it can become chronic (long-term), requiring more intensive treatment. Achilles tendonitis can also increase the risk of sustaining an Achilles tendon rupture (tear).
The Achilles tendon connects the calf muscles in the lower leg to the heel bone. It is the largest yet most exposed tendon in the body. Achilles tendonitis is where the Achilles tendon, and sometimes the protective sheath through which it moves, becomes inflamed, causing pain and swelling symptoms. Achilles tendonitis (also known as Achilles tendinopathy or tendonosis) is classified as an overuse injury. If left untreated it can become chronic (long-term), requiring more intensive treatment. Achilles tendonitis can also increase the risk of sustaining an Achilles tendon rupture (tear).
Causes
Short of a trauma, the primary cause of Achilles tendonitis is when the calf muscle is so tight that the heel is unable to come down to the ground placing extreme stress on the Achilles tendon at the insertion. Keep in mind that the calf muscle is designed to contract up, lifting the heel bone off the ground, propelling you forwards to the front of the foot for push off. When the calf is so tight that the heel is prevented from coming down on the ground there will be stress on the tendon and the foot will over pronate causing the Achilles tendon to twist, adding to the stress on the insertion. Improper treatment may lead to a more severe injury, such as a rupture or chronic weakening, which may require surgery.
Symptoms
Symptoms vary because you can injure various areas of the muscle-tendon complex. The pain may be an acute or chronic sharp, stabbing, piercing, shooting, burning or aching. It is often most noticeable immediately after getting out of bed in the morning, or after periods of inactivity, like sitting down for lunch. After a couple minutes of walking around, it will often then settle down somewhat, before becoming symptomatic again after excessive time standing or walking. But regardless of how the pain is perceived, Achilles tendon pain should not be left untreated due to the danger that the tendon can become weak, frayed, thickened, and eventually it may rupture.
Diagnosis
A doctor or professional therapist will confirm a diagnosis, identify and correct possible causes, apply treatment and prescribe eccentric rehabilitation exercises. An MRI or Ultrasound scan can determine the extent of the injury and indicate a precise diagnosis. Gait analysis along with a physical assessment will identify any possible biomechanical factors such as over pronation which may have contributed to the achilles tendonitis and training methods will be considered. Biomechanical problems can be corrected with the use of orthotic inserts and selection of correct footwear.
Nonsurgical Treatment
Massage therapy improves blood flow to the muscles and tissues of the affected area while increasing range of motion and can prevent recurring injury. The healing process can be quickened using ultrasound heat therapy to improve blood flow to the affected area. Wearing a night brace keeps the leg flexed, preventing stiffening of the tendon, which would impair healing. Stretching exercises increase flexibility and allow the tendon to heal without shortening, a deformity resulting in chronic pain. Persistent Achilles pain may warrant the use of a cast or walking boot to be worn for 4-6 weeks stabilizing the tendon so it can heal. After removal of the cast or boot, physical therapy will be ordered to increase functionality of the affected limb. To reduce chronic inflammation of the tendon, corticosteroid injections may be prescribed. It?s important to note that this corticosteroid treatment increases the risk of tendon rupture. Ultrasound imaging may be used by the physician administering the steroid injection, in order to help visualize the affected area. When all other therapies have failed to or tendon rupture occurs, surgical intervention and repair of the muscles and tendons is the last treatment option.

Surgical Treatment
If non-surgical approaches fail to restore the tendon to its normal condition, surgery may be necessary. The foot and ankle surgeon will select the best procedure to repair the tendon, based upon the extent of the injury, the patient?s age and activity level, and other factors.
Prevention
As with all injuries, prevention is your best defense especially with injuries that are as painful and inconvenient as Achilles tendonitis. Options for how to prevent Achilles tendonitis include, stretching- Stretching properly, starting slowly, and increasing gradually will be critical if you want to avoid Achilles tendonitis. To help maintain flexibility in the ankle joint, begin each day with a series of stretches and be certain to stretch prior to, and after, any exercise or excessive physical activity. Orthotics and Heel Support- Bio-mechanically engineered inserts and heel cups can be placed in your shoes to correct misalignments or bolster the support of your foot and are available without a prescription. The temporary heel padding that these provide reduces the length that the Achilles tendon stretches each time you step, making it more comfortable to go about your daily routine. Proper Footwear- Low-heeled shoes with good arch support and shock absorption are best for the health of your foot. Look into heel wedges and other shoe inserts to make sure that your everyday foot mechanics are operating under ideal conditions.
What Could Cause Arch Pain ?
Overview
Ligaments in the foot hold the muscle and bone structure in its arch shape, additionally supported by sinewy tissue. When these ligaments are torn, or when the bones are fractured, arch pain can be caused the by the incongruity of the interactivity of these different foot structures. Pain is the primary symptom of arch injuries, as well as general foot tenderness and increased difficulty in walking, running, and other otherwise normal foot movements.

Causes
Stress fractures, plantar fasciitis, and acute and chronic arthritis are most commonly the result of repetitive micro-trauma injuries. Micro-trauma injuries are caused when the structures of the body are stressed and re-stressed to the point that damage occurs in the tissues. Factors that commonly contribute to this injury can be running on uneven surfaces or surfaces that are too hard or too soft, shoes that have poor force-absorption qualities, or going too hard or too long during repeated exercise bouts.
Symptoms
Go to a podiatrist at the first sign of symptoms. Besides pain on the bottom of the foot, additional symptoms may include burning sensation in arch, difficulty standing on tiptoes, inflammation, more pain after sleeping or resting, redness, heat, localized pain in the ball of the foot, sharp or shooting pain in the toes, pain that increases when toes are flexed, tingling or numbness in the toes, aching, pain that increases when walking barefoot, pain that increases when walking on hard surfaces, pain the increases when standing (putting weight on your feet) or moving around and decreases when immobile, skin Lesions, it?s important to get a proper diagnosis and treatment plan. Let?s go over the possible causes of the pain.
Diagnosis
In more difficult cases of plantar fasciitis you should see your foot health professional for a thorough examination. They will find out why your arch or heel pain occurred in the first place and devise a treatment plan to relieve your pain and prevent it from reoccurring. They will evaluate your feet, walking pattern (gait), shoes, activities, exercise methods, and other relevant information and then devise your treatment plan.
Non Surgical Treatment
Treatment of plantar fasciitis is sometimes a drawn out and frustrating process. A program of rehabilitation should be undertaken with the help of someone qualified and knowledgeable about the affliction. Typically, plantar fasciitis will require at least six weeks and up to six months of conservative care to be fully remedied. Should such efforts not provide relief to the athlete, more aggressive measures including surgery may be considered. The initial goals of physical therapy should be to increase the passive flexion of the foot and improve flexibility in the foot and ankle, eventually leading to a full return to normal function. Prolonged inactivity in vigorous sports is often the price to be paid for thorough recovery. Half measures can lead to a chronic condition, in some cases severely limiting athletic ability.

Surgical Treatment
Surgery for flat feet is separated into three kinds: soft tissue procedures, bone cuts, and bone fusions. Depending on the severity of the flat foot, a person?s age, and whether or not the foot is stiff determines just how the foot can be fixed. In most cases a combination of procedures are performed. With flexible flat feet, surgery is geared at maintaining the motion of the foot and recreating the arch. Commonly this may involve tendon repairs along the inside of the foot to reinforce the main tendon that lifts the arch. When the bone collapse is significant, bone procedures are included to physically rebuild the arch, and realign the heel. The presence of bunions with flat feet is often contributing to the collapse and in most situations requires correction. With rigid flat feet, surgery is focused on restoring the shape of the foot through procedures that eliminate motion. In this case, motion does not exist pre-operatively, so realigning the foot is of utmost importance. The exception, are rigid flat feet due to tarsal coalition (fused segment of bone) in the back of the foot where freeing the blockage can restore function.
Prevention
People who run regularly should replace shoes every six months, more frequently if an avid runner. Avoid running or stepping on uneven surfaces. Try to be careful on rocky terrain or hills with loose gravel. Holes, tree stumps and roots are problems if you are trail running. If you have problems with the lower legs, a dirt road is softer than asphalt, which is softer than concrete. Try to pick a good surface if possible. However, if you're racing, be sure to train on the surface you'll eventually run on. Be careful running too many hills. Running uphill is a great workout, but make sure you gradually build this up to avoid injuries. Be careful when running downhill too fast, which can often lead to more injuries than running uphills. Prevent recurrent injuries. Athletes who have experienced ankle injuries previously may benefit from using a brace or tape to prevent recurrent ankle injuries.
Stretching Exercises
You may start exercising the muscles of your foot right away by gently stretching and strengthening them. Frozen can roll. Roll your bare injured foot back and forth from your heel to your mid-arch over a frozen juice can. Repeat for 3 to 5 minutes. This exercise is particularly helpful if it is done first thing in the morning. Towel stretch. Sit on a hard surface with your injured leg stretched out in front of you. Loop a towel around your toes and the ball of your foot and pull the towel toward your body keeping your leg straight. Hold this position for 15 to 30 seconds and then relax. Repeat 3 times. Standing calf stretch. Stand facing a wall with your hands on the wall at about eye level. Keep your injured leg back with your heel on the floor. Keep the other leg forward with the knee bent. Turn your back foot slightly inward (as if you were pigeon-toed). Slowly lean into the wall until you feel a stretch in the back of your calf. Hold the stretch for 15 to 30 seconds. Return to the starting position. Repeat 3 times. Do this exercise several times each day. Seated plantar fascia stretch. Sit in a chair and cross the injured foot over the knee of your other leg. Place your fingers over the base of your toes and pull them back toward your shin until you feel a comfortable stretch in the arch of your foot. Hold 15 seconds and repeat 3 times. Plantar fascia massage. Sit in a chair and cross the injured foot over the knee of your other leg. Place your fingers over the base of the toes of your injured foot and pull your toes toward your shin until you feel a stretch in the arch of your foot. With your other hand, massage the bottom of your foot, moving from the heel toward your toes. Do this for 3 to 5 minutes. Start gently. Press harder on the bottom of your foot as you become able to tolerate more pressure.
Ligaments in the foot hold the muscle and bone structure in its arch shape, additionally supported by sinewy tissue. When these ligaments are torn, or when the bones are fractured, arch pain can be caused the by the incongruity of the interactivity of these different foot structures. Pain is the primary symptom of arch injuries, as well as general foot tenderness and increased difficulty in walking, running, and other otherwise normal foot movements.

Causes
Stress fractures, plantar fasciitis, and acute and chronic arthritis are most commonly the result of repetitive micro-trauma injuries. Micro-trauma injuries are caused when the structures of the body are stressed and re-stressed to the point that damage occurs in the tissues. Factors that commonly contribute to this injury can be running on uneven surfaces or surfaces that are too hard or too soft, shoes that have poor force-absorption qualities, or going too hard or too long during repeated exercise bouts.
Symptoms
Go to a podiatrist at the first sign of symptoms. Besides pain on the bottom of the foot, additional symptoms may include burning sensation in arch, difficulty standing on tiptoes, inflammation, more pain after sleeping or resting, redness, heat, localized pain in the ball of the foot, sharp or shooting pain in the toes, pain that increases when toes are flexed, tingling or numbness in the toes, aching, pain that increases when walking barefoot, pain that increases when walking on hard surfaces, pain the increases when standing (putting weight on your feet) or moving around and decreases when immobile, skin Lesions, it?s important to get a proper diagnosis and treatment plan. Let?s go over the possible causes of the pain.
Diagnosis
In more difficult cases of plantar fasciitis you should see your foot health professional for a thorough examination. They will find out why your arch or heel pain occurred in the first place and devise a treatment plan to relieve your pain and prevent it from reoccurring. They will evaluate your feet, walking pattern (gait), shoes, activities, exercise methods, and other relevant information and then devise your treatment plan.
Non Surgical Treatment
Treatment of plantar fasciitis is sometimes a drawn out and frustrating process. A program of rehabilitation should be undertaken with the help of someone qualified and knowledgeable about the affliction. Typically, plantar fasciitis will require at least six weeks and up to six months of conservative care to be fully remedied. Should such efforts not provide relief to the athlete, more aggressive measures including surgery may be considered. The initial goals of physical therapy should be to increase the passive flexion of the foot and improve flexibility in the foot and ankle, eventually leading to a full return to normal function. Prolonged inactivity in vigorous sports is often the price to be paid for thorough recovery. Half measures can lead to a chronic condition, in some cases severely limiting athletic ability.

Surgical Treatment
Surgery for flat feet is separated into three kinds: soft tissue procedures, bone cuts, and bone fusions. Depending on the severity of the flat foot, a person?s age, and whether or not the foot is stiff determines just how the foot can be fixed. In most cases a combination of procedures are performed. With flexible flat feet, surgery is geared at maintaining the motion of the foot and recreating the arch. Commonly this may involve tendon repairs along the inside of the foot to reinforce the main tendon that lifts the arch. When the bone collapse is significant, bone procedures are included to physically rebuild the arch, and realign the heel. The presence of bunions with flat feet is often contributing to the collapse and in most situations requires correction. With rigid flat feet, surgery is focused on restoring the shape of the foot through procedures that eliminate motion. In this case, motion does not exist pre-operatively, so realigning the foot is of utmost importance. The exception, are rigid flat feet due to tarsal coalition (fused segment of bone) in the back of the foot where freeing the blockage can restore function.
Prevention
People who run regularly should replace shoes every six months, more frequently if an avid runner. Avoid running or stepping on uneven surfaces. Try to be careful on rocky terrain or hills with loose gravel. Holes, tree stumps and roots are problems if you are trail running. If you have problems with the lower legs, a dirt road is softer than asphalt, which is softer than concrete. Try to pick a good surface if possible. However, if you're racing, be sure to train on the surface you'll eventually run on. Be careful running too many hills. Running uphill is a great workout, but make sure you gradually build this up to avoid injuries. Be careful when running downhill too fast, which can often lead to more injuries than running uphills. Prevent recurrent injuries. Athletes who have experienced ankle injuries previously may benefit from using a brace or tape to prevent recurrent ankle injuries.
Stretching Exercises
You may start exercising the muscles of your foot right away by gently stretching and strengthening them. Frozen can roll. Roll your bare injured foot back and forth from your heel to your mid-arch over a frozen juice can. Repeat for 3 to 5 minutes. This exercise is particularly helpful if it is done first thing in the morning. Towel stretch. Sit on a hard surface with your injured leg stretched out in front of you. Loop a towel around your toes and the ball of your foot and pull the towel toward your body keeping your leg straight. Hold this position for 15 to 30 seconds and then relax. Repeat 3 times. Standing calf stretch. Stand facing a wall with your hands on the wall at about eye level. Keep your injured leg back with your heel on the floor. Keep the other leg forward with the knee bent. Turn your back foot slightly inward (as if you were pigeon-toed). Slowly lean into the wall until you feel a stretch in the back of your calf. Hold the stretch for 15 to 30 seconds. Return to the starting position. Repeat 3 times. Do this exercise several times each day. Seated plantar fascia stretch. Sit in a chair and cross the injured foot over the knee of your other leg. Place your fingers over the base of your toes and pull them back toward your shin until you feel a comfortable stretch in the arch of your foot. Hold 15 seconds and repeat 3 times. Plantar fascia massage. Sit in a chair and cross the injured foot over the knee of your other leg. Place your fingers over the base of the toes of your injured foot and pull your toes toward your shin until you feel a stretch in the arch of your foot. With your other hand, massage the bottom of your foot, moving from the heel toward your toes. Do this for 3 to 5 minutes. Start gently. Press harder on the bottom of your foot as you become able to tolerate more pressure.
Does Pain In The Arch Require Surgical Treatment ?
Overview
The arch functions as a shock absorber for our entire body. Each time we step down, we place up to 5 times our body weight on the foot, depending on whether we are walking, running, or jumping. If there were no shock absorber in the foot, the force of each step would fracture or dislocate the bones of the foot, leg, and lower back. When pain occurs in the arch, it is telling us it is "sick" and cannot function properly. If left untreated, it can cause constant pain throughout the entire foot, and eventually the knee, hip, and lower back.

Causes
Arch and heel pain is usually the result of faulty biomechanics (walking gait abnormalities) that place too much stress on the heel bone and the soft tissues that attach to it. This increased stress causes local inflammation and pain. The most common cause of the stress is a condition where the inside arch of the foot flattens more than it should (often known as "over-pronation"). When the arch of the foot flattens, it also gets longer, causing a stretch on the plantar fascia. In response, the heel becomes inflamed where the plantar fascia attaches.
Symptoms
Typically, the sufferer of plantar fasciitis experiences pain upon rising after sleep, particularly the first step out of bed. Such pain is tightly localized at the bony landmark on the anterior medial tubercle of the calcaneus. In some cases, pain may prevent the athlete from walking in a normal heel-toe gait, causing an irregular walk as means of compensation. Less common areas of pain include the forefoot, Achilles tendon, or subtalar joint. After a brief period of walking, the pain usually subsides, but returns again either with vigorous activity or prolonged standing or walking. On the field, an altered gait or abnormal stride pattern, along with pain during running or jumping activities are tell-tale signs of plantar fasciitis and should be given prompt attention. Further indications of the injury include poor dorsiflexion (lifting the forefoot off the ground) due to a shortened gastroc complex, (muscles of the calf). Crouching in a full squat position with the sole of the foot flat on the ground can be used as a test, as pain will preclude it for the athlete suffering from plantar fasciitis, causing an elevation of the heel due to tension in the gastroc complex.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
Non Surgical Treatment
If it is flat feet, then you'd seek professional advice and maybe need orthotics, or arch supports to prevent the pressures and to stop the pain. One of the other reasons you can get pain in this area of the foot is plantar fasciitis. The plantar fascia is a membrane that is inside of the skin and attaches to the heel bone here. It divides into three bands that go out of the foot here: the outer band, the central band, and the medial band here. Often, from impact, you get an inflammation of that attachment to the heel bone and this can often spread up the medial band and this is another way of getting pain in that arch. Now, the way to treat that is also using arch supports but also heel cushions, better soled shoes to prevent the pressure. These things normally disappear after a year, 18 months. Plantar fasciitis is easier to treat because it's not a long term problem. If you do need arch support, something like this would be very good for both problems.

Surgical Treatment
The main goal of surgery is to reduce pain and improve function. It may also reduce other injuries such as repeated ankle sprains and broken bones. Surgery may be considered if there is no relief with physical therapy, changes in shoewear and/or changes in activity. Some patients will also have tendon problems, ankle weakness and foot fractures. These patients may require other procedures to address related problems. If you have medical problems that make surgery unsafe, any infections or blood vessel disease, cavus foot surgery may not be appropriate. The surgical procedures involved with the correction of the cavus foot are varied. Theses may include correction of the bony deformity, ankle looseness and the muscle imbalances that cause the deformity. The goal is to provide a foot that evenly distributes weight along both inside and outside edges. A variety of incisions may be needed to perform the procedures related to the correction of the cavus foot.
Prevention
Strap the arches into the anatomically correct positions with athletic tape and leave them like this for some time. If the fallen arches are an issue with the muscular structure, this may give the muscles an opportunity to strengthen. This is definitely not a fallen arches cure all the time but it can help prevent it more times than not. Ask a doctor or physical therapists to show you how to do this taping. Find shoes that fit. This may require that you get your foot measured and molded to ensure that the shoe will fit. Shoes that are too big, too tight or too short, may not directly cause the fallen arches, but they can assist with the damage to the area. These shoes should have thick cushioning inside and have plenty of room for your toes. Walk without shoes as much as possible. Shoes directly assist with weakening and distorting the arches of the feet so going without shoes can actually help strengthen your arches and prevent fallen arches. Walking on hard and bumpy surfaces barefooted makes the muscles in your feet strengthen in order to prevent injury. It is a coping mechanism by your body. Insert heel cups or insoles into the shoes that you wear the most. Many people wear uncomfortable shoes to work and these are the same shoes that cause their arches the most problems. Inserting the heel cups and insoles into these shoes can prevent fallen arches from occurring. Many people place these inserts into all their shoes to ensure support. Ask a medical professional, either your doctor or a physical therapist, about daily foot exercises that may keep the arches stronger than normal. Many times, you can find exercises and stretches on the Internet on various websites. Curling your toes tightly and rotating your feet will help strengthen your longitudinal arches. Relax your feet and shake them for a minute or so before you do any arch exercises. This will loosen the muscles in your feet that stay tight due to normal daily activities. Wear rigid soled sandals whenever possible to provide a strong support for your arches. Wooden soled sandals are the best ones if available. Walk or jog on concrete as much as you can. This will create a sturdy support for your arches. Running or walking in sandy areas or even on a treadmill, does not give rigid support. Instead, these surfaces absorb the step, offering no support for arches.
The arch functions as a shock absorber for our entire body. Each time we step down, we place up to 5 times our body weight on the foot, depending on whether we are walking, running, or jumping. If there were no shock absorber in the foot, the force of each step would fracture or dislocate the bones of the foot, leg, and lower back. When pain occurs in the arch, it is telling us it is "sick" and cannot function properly. If left untreated, it can cause constant pain throughout the entire foot, and eventually the knee, hip, and lower back.

Causes
Arch and heel pain is usually the result of faulty biomechanics (walking gait abnormalities) that place too much stress on the heel bone and the soft tissues that attach to it. This increased stress causes local inflammation and pain. The most common cause of the stress is a condition where the inside arch of the foot flattens more than it should (often known as "over-pronation"). When the arch of the foot flattens, it also gets longer, causing a stretch on the plantar fascia. In response, the heel becomes inflamed where the plantar fascia attaches.
Symptoms
Typically, the sufferer of plantar fasciitis experiences pain upon rising after sleep, particularly the first step out of bed. Such pain is tightly localized at the bony landmark on the anterior medial tubercle of the calcaneus. In some cases, pain may prevent the athlete from walking in a normal heel-toe gait, causing an irregular walk as means of compensation. Less common areas of pain include the forefoot, Achilles tendon, or subtalar joint. After a brief period of walking, the pain usually subsides, but returns again either with vigorous activity or prolonged standing or walking. On the field, an altered gait or abnormal stride pattern, along with pain during running or jumping activities are tell-tale signs of plantar fasciitis and should be given prompt attention. Further indications of the injury include poor dorsiflexion (lifting the forefoot off the ground) due to a shortened gastroc complex, (muscles of the calf). Crouching in a full squat position with the sole of the foot flat on the ground can be used as a test, as pain will preclude it for the athlete suffering from plantar fasciitis, causing an elevation of the heel due to tension in the gastroc complex.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
Non Surgical Treatment
If it is flat feet, then you'd seek professional advice and maybe need orthotics, or arch supports to prevent the pressures and to stop the pain. One of the other reasons you can get pain in this area of the foot is plantar fasciitis. The plantar fascia is a membrane that is inside of the skin and attaches to the heel bone here. It divides into three bands that go out of the foot here: the outer band, the central band, and the medial band here. Often, from impact, you get an inflammation of that attachment to the heel bone and this can often spread up the medial band and this is another way of getting pain in that arch. Now, the way to treat that is also using arch supports but also heel cushions, better soled shoes to prevent the pressure. These things normally disappear after a year, 18 months. Plantar fasciitis is easier to treat because it's not a long term problem. If you do need arch support, something like this would be very good for both problems.

Surgical Treatment
The main goal of surgery is to reduce pain and improve function. It may also reduce other injuries such as repeated ankle sprains and broken bones. Surgery may be considered if there is no relief with physical therapy, changes in shoewear and/or changes in activity. Some patients will also have tendon problems, ankle weakness and foot fractures. These patients may require other procedures to address related problems. If you have medical problems that make surgery unsafe, any infections or blood vessel disease, cavus foot surgery may not be appropriate. The surgical procedures involved with the correction of the cavus foot are varied. Theses may include correction of the bony deformity, ankle looseness and the muscle imbalances that cause the deformity. The goal is to provide a foot that evenly distributes weight along both inside and outside edges. A variety of incisions may be needed to perform the procedures related to the correction of the cavus foot.
Prevention
Strap the arches into the anatomically correct positions with athletic tape and leave them like this for some time. If the fallen arches are an issue with the muscular structure, this may give the muscles an opportunity to strengthen. This is definitely not a fallen arches cure all the time but it can help prevent it more times than not. Ask a doctor or physical therapists to show you how to do this taping. Find shoes that fit. This may require that you get your foot measured and molded to ensure that the shoe will fit. Shoes that are too big, too tight or too short, may not directly cause the fallen arches, but they can assist with the damage to the area. These shoes should have thick cushioning inside and have plenty of room for your toes. Walk without shoes as much as possible. Shoes directly assist with weakening and distorting the arches of the feet so going without shoes can actually help strengthen your arches and prevent fallen arches. Walking on hard and bumpy surfaces barefooted makes the muscles in your feet strengthen in order to prevent injury. It is a coping mechanism by your body. Insert heel cups or insoles into the shoes that you wear the most. Many people wear uncomfortable shoes to work and these are the same shoes that cause their arches the most problems. Inserting the heel cups and insoles into these shoes can prevent fallen arches from occurring. Many people place these inserts into all their shoes to ensure support. Ask a medical professional, either your doctor or a physical therapist, about daily foot exercises that may keep the arches stronger than normal. Many times, you can find exercises and stretches on the Internet on various websites. Curling your toes tightly and rotating your feet will help strengthen your longitudinal arches. Relax your feet and shake them for a minute or so before you do any arch exercises. This will loosen the muscles in your feet that stay tight due to normal daily activities. Wear rigid soled sandals whenever possible to provide a strong support for your arches. Wooden soled sandals are the best ones if available. Walk or jog on concrete as much as you can. This will create a sturdy support for your arches. Running or walking in sandy areas or even on a treadmill, does not give rigid support. Instead, these surfaces absorb the step, offering no support for arches.
The Treatments and Causes
Overview
Adult acquired flatfoot deformity or even posterior tibial tendon dysfunction is a gradual however progressive loss associated with ones arch. Your posterior tibial muscle mass is a deep muscle mass within the back with the calf. That features a extended tendon that extends coming from higher than the ankle as well as attaches directly into several sites around the arch with the foot. The Actual muscle acts just like a stirrup about the inside of the foot to aid keep the arch. Your posterior tibial muscle mass stabilizes the arch along with produces a rigid platform with regard to walking and also running. In case the particular posterior tibial tendon gets to be able to be damaged or even tears the arch loses its stability so that as a result, collapses causing a flatfoot. Adult flatfoot deformity may appear in individuals of most ages and gender however, it occurs mostly within sedentary middle older to elderly females. You will find several risk elements with regard to posterior tibial tendon dysfunction that will include: obesity, steroid use, systemic inflammatory diseases such as rheumatoid arthritis, trauma, becoming born having a reduced arch, along with diabetes. The idea occurs mostly in a foot however, it can occur in each feet particularly in individuals with systemic diseases such as diabetes and rheumatoid arthritis.

Causes
Many wellness conditions may produce a painful flatfoot, a individual injury to the ligaments within the foot could cause your joints for you to fall from alignment. The Particular ligaments keep the bones and stop them through moving. When the ligaments are usually torn, the particular foot will become flat along with painful. This specific more generally occurs in the core foot (Lisfranc injury), but tend to additionally occur inside the back again of the foot. Additionally for you to ligament injuries, fractures as well as dislocations with the bones in the midfoot can easily also cause a flatfoot deformity.
Symptoms
The the indicators of PTTD can include pain, swelling, the flattening with the arch, and an inward rolling in the ankle. Since the particular condition progresses, the signs along with symptoms will change. Pertaining To example, when PTTD initially develops, there is pain around the inside with the foot as well as ankle (along the span of the particular tendon). in addition, the region may become red, warm, along with swollen. Later, as the arch begins to flatten, there could be pain about the inside in the foot along with ankle. However at this point, the actual foot as well as toes begin to turn outward and the ankle rolls inward. Since PTTD gets to become more advanced, the actual arch flattens even more and the pain usually shifts for the outside the foot, under the ankle. The Particular tendon provides deteriorated considerably and arthritis often develops within the foot. Inside a lot more severe cases, arthritis might also develop in the ankle.
Diagnosis
Diagnostic testing can be usually used to diagnose the situation as well as assist figure out happens of the disease. The Particular most common test done in the workplace setting tend to be weightbearing X-rays in the foot and ankle. These assess joint alignment and osteoarthritis. When tendon tearing as well as rupture can be suspected, the actual gold standard test could be MRI. The Actual MRI is actually accustomed to verify the actual tendon, surrounding ligament structures and in addition the midfoot and also hindfoot joints. An MRI is essential if surgery can be being considered.
Non surgical Treatment
Because with the progressive naturel of PTTD, early remedy is actually critical. In case handled quickly enough, signs might resolve without having the actual dependence on surgery and progression in the condition could be stopped. In the particular event that left untreated, PTTD might create an very flat foot, painful arthritis in the foot as well as ankle, and can restrict the power to walk, run, along together with other activities. The podiatrist might recommend one as well as really these non-surgical therapies to become able to manage the PTTD. Orthotic devices or bracing. to give your current arch the actual assistance it needs, your current foot and ankle surgeon may recommend an ankle brace or even a custom orthotic device that matches in your shoe for you to offer the arch. Immobilization. The short-leg cast or even boot may be worn for you to immobilize the particular foot and enable the particular tendon for you to heal. Bodily therapy. Ultrasound therapy and stretching workouts may help rehabilitate the particular tendon as well as muscle following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), for example ibuprofen, help decrease the pain as well as inflammation. Shoe modifications. your foot as well as ankle surgeon may recommend changes within your footwear.

Surgical Treatment
When conservative treatment does not control signs along with symptoms and/or deformity, then surgery could end up being needed. Your objective of surgical therapy is to obtain excellent alignment while keeping the particular foot and also ankle as flexible as possible. the most common procedures used with this condition contain arthrodesis (fusion), osteotomy (cutting out the wedge-shaped little bit of bone), as well as lateral column lengthening. Lateral column lengthening necessitates the use of a bone graft at the calcaneocuboid joint. This particular procedure helps restore your medial longitudinal arch (arch along the inside in the foot). A New torn tendon or perhaps spring ligament will most likely be repaired as well as reconstructed. Some Other surgical options contain tendon shortening as well as lengthening. As Well As the particular surgeon may transfer 1 or even more tendons. This specific procedure is actually known as the tendon transfer. Tendon transfer uses an additional tendon to aid the particular posterior tibial tendon perform much more effectively. A New tendon transfer can be made to alter the force and angle of pull around the bones of the arch. It's not necessarily obvious but coming from analysis evidence which usually surgical procedure works best for this condition. Any combination of surgical remedies might end up being needed. The idea could rely in your age, type along with severity of deformity along with symptoms, as well as your desired degree of day-to-day activity.
Adult acquired flatfoot deformity or even posterior tibial tendon dysfunction is a gradual however progressive loss associated with ones arch. Your posterior tibial muscle mass is a deep muscle mass within the back with the calf. That features a extended tendon that extends coming from higher than the ankle as well as attaches directly into several sites around the arch with the foot. The Actual muscle acts just like a stirrup about the inside of the foot to aid keep the arch. Your posterior tibial muscle mass stabilizes the arch along with produces a rigid platform with regard to walking and also running. In case the particular posterior tibial tendon gets to be able to be damaged or even tears the arch loses its stability so that as a result, collapses causing a flatfoot. Adult flatfoot deformity may appear in individuals of most ages and gender however, it occurs mostly within sedentary middle older to elderly females. You will find several risk elements with regard to posterior tibial tendon dysfunction that will include: obesity, steroid use, systemic inflammatory diseases such as rheumatoid arthritis, trauma, becoming born having a reduced arch, along with diabetes. The idea occurs mostly in a foot however, it can occur in each feet particularly in individuals with systemic diseases such as diabetes and rheumatoid arthritis.

Causes
Many wellness conditions may produce a painful flatfoot, a individual injury to the ligaments within the foot could cause your joints for you to fall from alignment. The Particular ligaments keep the bones and stop them through moving. When the ligaments are usually torn, the particular foot will become flat along with painful. This specific more generally occurs in the core foot (Lisfranc injury), but tend to additionally occur inside the back again of the foot. Additionally for you to ligament injuries, fractures as well as dislocations with the bones in the midfoot can easily also cause a flatfoot deformity.
Symptoms
The the indicators of PTTD can include pain, swelling, the flattening with the arch, and an inward rolling in the ankle. Since the particular condition progresses, the signs along with symptoms will change. Pertaining To example, when PTTD initially develops, there is pain around the inside with the foot as well as ankle (along the span of the particular tendon). in addition, the region may become red, warm, along with swollen. Later, as the arch begins to flatten, there could be pain about the inside in the foot along with ankle. However at this point, the actual foot as well as toes begin to turn outward and the ankle rolls inward. Since PTTD gets to become more advanced, the actual arch flattens even more and the pain usually shifts for the outside the foot, under the ankle. The Particular tendon provides deteriorated considerably and arthritis often develops within the foot. Inside a lot more severe cases, arthritis might also develop in the ankle.
Diagnosis
Diagnostic testing can be usually used to diagnose the situation as well as assist figure out happens of the disease. The Particular most common test done in the workplace setting tend to be weightbearing X-rays in the foot and ankle. These assess joint alignment and osteoarthritis. When tendon tearing as well as rupture can be suspected, the actual gold standard test could be MRI. The Actual MRI is actually accustomed to verify the actual tendon, surrounding ligament structures and in addition the midfoot and also hindfoot joints. An MRI is essential if surgery can be being considered.
Non surgical Treatment
Because with the progressive naturel of PTTD, early remedy is actually critical. In case handled quickly enough, signs might resolve without having the actual dependence on surgery and progression in the condition could be stopped. In the particular event that left untreated, PTTD might create an very flat foot, painful arthritis in the foot as well as ankle, and can restrict the power to walk, run, along together with other activities. The podiatrist might recommend one as well as really these non-surgical therapies to become able to manage the PTTD. Orthotic devices or bracing. to give your current arch the actual assistance it needs, your current foot and ankle surgeon may recommend an ankle brace or even a custom orthotic device that matches in your shoe for you to offer the arch. Immobilization. The short-leg cast or even boot may be worn for you to immobilize the particular foot and enable the particular tendon for you to heal. Bodily therapy. Ultrasound therapy and stretching workouts may help rehabilitate the particular tendon as well as muscle following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), for example ibuprofen, help decrease the pain as well as inflammation. Shoe modifications. your foot as well as ankle surgeon may recommend changes within your footwear.

Surgical Treatment
When conservative treatment does not control signs along with symptoms and/or deformity, then surgery could end up being needed. Your objective of surgical therapy is to obtain excellent alignment while keeping the particular foot and also ankle as flexible as possible. the most common procedures used with this condition contain arthrodesis (fusion), osteotomy (cutting out the wedge-shaped little bit of bone), as well as lateral column lengthening. Lateral column lengthening necessitates the use of a bone graft at the calcaneocuboid joint. This particular procedure helps restore your medial longitudinal arch (arch along the inside in the foot). A New torn tendon or perhaps spring ligament will most likely be repaired as well as reconstructed. Some Other surgical options contain tendon shortening as well as lengthening. As Well As the particular surgeon may transfer 1 or even more tendons. This specific procedure is actually known as the tendon transfer. Tendon transfer uses an additional tendon to aid the particular posterior tibial tendon perform much more effectively. A New tendon transfer can be made to alter the force and angle of pull around the bones of the arch. It's not necessarily obvious but coming from analysis evidence which usually surgical procedure works best for this condition. Any combination of surgical remedies might end up being needed. The idea could rely in your age, type along with severity of deformity along with symptoms, as well as your desired degree of day-to-day activity.
Will Adult Aquired FlatFoot Require Surgery Teatment ?
Overview
Adult acquired flatfoot deformity or even posterior tibial tendon dysfunction can be a gradual however progressive loss regarding ones arch. Your posterior tibial muscle is truly a deep muscle mass inside the back again in the calf. It features a long tendon that extends coming from above the ankle as well as attaches directly into a range of websites across the arch with the foot. The Actual muscle mass acts like a stirrup about the inside of the foot to aid offer the arch. the posterior tibial muscle stabilizes the arch along with produces a rigid platform pertaining to walking as well as running. In case the actual posterior tibial tendon gets in order to be damaged or even tears your arch loses its stability and as the result, collapses causing any flatfoot. Adult flatfoot deformity may occur in folks of all ages as well as gender however, it occurs most commonly in sedentary middle aged in order to elderly females. You can find numerous risk elements pertaining to posterior tibial tendon dysfunction in which include: obesity, steroid use, systemic inflammatory diseases like rheumatoid arthritis, trauma, getting born with a lower arch, as well as diabetes. That occurs most commonly in a foot however, it may exist in each feet specifically in individuals with systemic diseases for example diabetes and rheumatoid arthritis.
Causes
Obesity - Overtime if your entire body is carrying those added pounds, you can potentially injure the feet. The Actual additional weight puts stress on the ligaments in which assistance the feet. Furthermore getting more than excess weight could lead to type two diabetes which in turn furthermore can easily attribute in order to AAFD. Diabetes - Diabetes could additionally play a role in Adult Acquired Flatfoot Deformity. Diabetes may cause injury to ligaments, which usually support the feet and other bones within your body. In addition to damaged ligaments, uncontrolled diabetes could result in ulcers in your feet. When the arches fall within the feet, the front with the foot can be wider, as well as outer aspects of your foot can learn to rub within your shoe wear. Patients along with uncontrolled diabetes might not notice or even have got symptoms of pain because of to be able to nerve damage. Diabetic patient don?t observe these people have a problem, along with other complications occur in the feet like ulcers as well as wounds. Hypertension - Substantial blood pressure trigger arteries narrow overtime, which usually could reduce blood flow in order to ligaments. The Actual blood flow towards the ligaments is exactly what keeps the foot arches healthy, along with supportive. Arthritis - Arthritis can form within an old injury overtime this could cause flatfeet as well. Arthritis is painful also which contributes towards the elevated pain involving AAFD. Injury - Injuries are a common purpose also for AAFD. Anxiety through impact sports. Ligament damage coming from injury can cause your bones of the foot to fallout involving ailment. Overtime the ligaments will tear and also result in complete flattening involving feet.
Symptoms
Your feet tire effortlessly or even grow to always be able to be painful together with prolonged standing. It's challenging to go the heel or midfoot around, or to stand on your toes. The foot aches, specially inside the heel or arch area, along with swelling across the inner side. Pain within your feet decreases your own power to participate in sports. You've been clinically determined to have rheumatoid arthritis; concerning 1 / two of just about all people with rheumatoid arthritis will develop a progressive flatfoot deformity.
Diagnosis
Starting from your knee down, check for virtually any bowing with the tibia. a tibial varum will trigger elevated medial tension about the foot and also ankle. This could be essential to contemplate inside surgical planning. Verify the actual gastrocnemius muscle mass and Achilles complex via a new straight as well as bent knee check with regard to equinus. When your array of motion improves for you to no less than neutral together with bent knee testing in the Achilles complex, one could think regarding a gastrocnemius recession. In case the actual Achilles complex is nevertheless tight using bent knee testing, an Achilles lengthening could become necessary. Examine your posterior tibial muscle along its entire course. Palpate the actual muscle mass and also observe the tendon regarding strength having a plantarflexion as well as inversion stress test. Examine the actual flexor muscles regarding strength to always be able to ascertain if a sufficient transfer tendon will be available. Verify your anterior tibial tendon regarding size along with strength.
Non surgical Treatment
Although AAF is not reversible with out surgery, appropriate treatment method should address the actual patient?s present symptoms, attempt to decrease pain, and enable continued ambulation. Inside your early stages, orthotic along with pedorthic solutions could address losing integrity in the foot?s support structures, potentially inhibiting further destruction.3-5 While a broad principle, orthotic devices ought to merely block as well as limit painful or destructive motion without having reducing or perhaps restricting normal motion as well as muscle function. Consequently, the therapy must match happens of the deformity.

Surgical Treatment
The indications pertaining to surgery are usually persistent pain and/or significant deformity. Occasionally the actual foot just feels weak and also the assessment involving deformity is nearly all beneficial carried out by a foot and also ankle specialist. In case surgery is actually appropriate, any mixture of soft tissue and bony treatments might end up being considered in order to right alignment and also offer the medial arch, using strain off failing ligaments. Depending upon the tissues concerned along with extent regarding deformity, the foot as well as ankle specialist will decide the actual necessary mixture of procedures. Surgical methods could include a medial slide calcaneal osteotomy in order to correct place with the heel, any lateral column lengthening to right place in the midfoot plus a medial cuneiform osteotomy as well as 1st metatarsal-tarsal fusion in order to correct elevation in the medial forefoot. Your posterior tibial tendon could end up being reconstructed using a tendon transfer. Within severe cases (stage III), the reconstruction can include fusion in the hind foot,, leading to stiffness with the hind foot however the desired pain relief. Throughout one with the most severe stage (stage IV), the deltoid ligament around the inside in the ankle fails, resulting in the deformity inside the ankle. This specific deformity over time may outcome in arthritis inside the ankle.
Adult acquired flatfoot deformity or even posterior tibial tendon dysfunction can be a gradual however progressive loss regarding ones arch. Your posterior tibial muscle is truly a deep muscle mass inside the back again in the calf. It features a long tendon that extends coming from above the ankle as well as attaches directly into a range of websites across the arch with the foot. The Actual muscle mass acts like a stirrup about the inside of the foot to aid offer the arch. the posterior tibial muscle stabilizes the arch along with produces a rigid platform pertaining to walking as well as running. In case the actual posterior tibial tendon gets in order to be damaged or even tears your arch loses its stability and as the result, collapses causing any flatfoot. Adult flatfoot deformity may occur in folks of all ages as well as gender however, it occurs most commonly in sedentary middle aged in order to elderly females. You can find numerous risk elements pertaining to posterior tibial tendon dysfunction in which include: obesity, steroid use, systemic inflammatory diseases like rheumatoid arthritis, trauma, getting born with a lower arch, as well as diabetes. That occurs most commonly in a foot however, it may exist in each feet specifically in individuals with systemic diseases for example diabetes and rheumatoid arthritis.
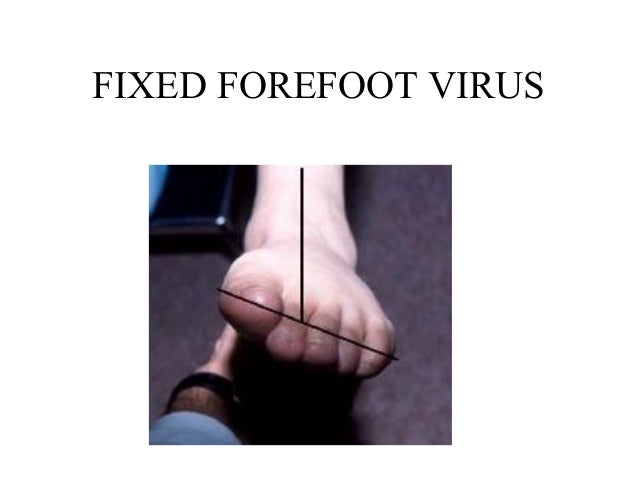
Causes
Obesity - Overtime if your entire body is carrying those added pounds, you can potentially injure the feet. The Actual additional weight puts stress on the ligaments in which assistance the feet. Furthermore getting more than excess weight could lead to type two diabetes which in turn furthermore can easily attribute in order to AAFD. Diabetes - Diabetes could additionally play a role in Adult Acquired Flatfoot Deformity. Diabetes may cause injury to ligaments, which usually support the feet and other bones within your body. In addition to damaged ligaments, uncontrolled diabetes could result in ulcers in your feet. When the arches fall within the feet, the front with the foot can be wider, as well as outer aspects of your foot can learn to rub within your shoe wear. Patients along with uncontrolled diabetes might not notice or even have got symptoms of pain because of to be able to nerve damage. Diabetic patient don?t observe these people have a problem, along with other complications occur in the feet like ulcers as well as wounds. Hypertension - Substantial blood pressure trigger arteries narrow overtime, which usually could reduce blood flow in order to ligaments. The Actual blood flow towards the ligaments is exactly what keeps the foot arches healthy, along with supportive. Arthritis - Arthritis can form within an old injury overtime this could cause flatfeet as well. Arthritis is painful also which contributes towards the elevated pain involving AAFD. Injury - Injuries are a common purpose also for AAFD. Anxiety through impact sports. Ligament damage coming from injury can cause your bones of the foot to fallout involving ailment. Overtime the ligaments will tear and also result in complete flattening involving feet.
Symptoms
Your feet tire effortlessly or even grow to always be able to be painful together with prolonged standing. It's challenging to go the heel or midfoot around, or to stand on your toes. The foot aches, specially inside the heel or arch area, along with swelling across the inner side. Pain within your feet decreases your own power to participate in sports. You've been clinically determined to have rheumatoid arthritis; concerning 1 / two of just about all people with rheumatoid arthritis will develop a progressive flatfoot deformity.
Diagnosis
Starting from your knee down, check for virtually any bowing with the tibia. a tibial varum will trigger elevated medial tension about the foot and also ankle. This could be essential to contemplate inside surgical planning. Verify the actual gastrocnemius muscle mass and Achilles complex via a new straight as well as bent knee check with regard to equinus. When your array of motion improves for you to no less than neutral together with bent knee testing in the Achilles complex, one could think regarding a gastrocnemius recession. In case the actual Achilles complex is nevertheless tight using bent knee testing, an Achilles lengthening could become necessary. Examine your posterior tibial muscle along its entire course. Palpate the actual muscle mass and also observe the tendon regarding strength having a plantarflexion as well as inversion stress test. Examine the actual flexor muscles regarding strength to always be able to ascertain if a sufficient transfer tendon will be available. Verify your anterior tibial tendon regarding size along with strength.
Non surgical Treatment
Although AAF is not reversible with out surgery, appropriate treatment method should address the actual patient?s present symptoms, attempt to decrease pain, and enable continued ambulation. Inside your early stages, orthotic along with pedorthic solutions could address losing integrity in the foot?s support structures, potentially inhibiting further destruction.3-5 While a broad principle, orthotic devices ought to merely block as well as limit painful or destructive motion without having reducing or perhaps restricting normal motion as well as muscle function. Consequently, the therapy must match happens of the deformity.

Surgical Treatment
The indications pertaining to surgery are usually persistent pain and/or significant deformity. Occasionally the actual foot just feels weak and also the assessment involving deformity is nearly all beneficial carried out by a foot and also ankle specialist. In case surgery is actually appropriate, any mixture of soft tissue and bony treatments might end up being considered in order to right alignment and also offer the medial arch, using strain off failing ligaments. Depending upon the tissues concerned along with extent regarding deformity, the foot as well as ankle specialist will decide the actual necessary mixture of procedures. Surgical methods could include a medial slide calcaneal osteotomy in order to correct place with the heel, any lateral column lengthening to right place in the midfoot plus a medial cuneiform osteotomy as well as 1st metatarsal-tarsal fusion in order to correct elevation in the medial forefoot. Your posterior tibial tendon could end up being reconstructed using a tendon transfer. Within severe cases (stage III), the reconstruction can include fusion in the hind foot,, leading to stiffness with the hind foot however the desired pain relief. Throughout one with the most severe stage (stage IV), the deltoid ligament around the inside in the ankle fails, resulting in the deformity inside the ankle. This specific deformity over time may outcome in arthritis inside the ankle.