Treating Calcaneal Apophysitis
Sever's Disease is a serious type of 'growing pain' rooted in the fact that the rate of growth of a child's heel bones is slower than that of the ligaments of the leg. The heel bone is one of the first bones in the human body to reach full size, and it is prone to injury because it is not flexible or elastic. As a child goes through growth spurts of the heel bone, the Achilles tendon, which connects the calf muscle to the heel, may be struggling to play catch-up, due to its slower rate of growth. In this scenario, the tendon and leg muscles can become strained, tight and over-stretched. As the child walks, runs or plays, repetitive pressure is placed on the tendon, and the tension can cause damage to the growing heel bone, resulting in pain and inflammation.
Causes
There is no specific known cause of Sever?s disease. However, there are several common factors associated with the condition including. Tight calf muscles. Pronated foot type (rolled in towards the ankle). Children who are heavier. Puberty/growth spurts. External factors, e.g. hard surfaces or poor footwear. Increase in physical activity levels.
Symptoms
The pain associated with Sever's disease is usually felt along the back of the heel and becomes worse when running or walking. In some children, the pain is so severe they may limp when walking. One of the diagnostic tests for Sever's disease is the "squeeze test". Squeezing both sides of the heel together will produce immediate discomfort. Many children feel pain immediately upon waking and may have calf muscle stiffness in the morning.
Diagnosis
You may have pain when your doctor squeezes your heel bone. You may have pain when asked to stand or walk on your toes or on your heels. You may have pain in your heel when your doctor stretches your calf muscles. Your doctor may order x-rays of the injured foot to show an active growth plate.
Non Surgical Treatment
Physiotherapy treatment to improve range of the ankle and descrease soft tissue tightness. Orthotics to control excessive motion of the foot. Icing the painful area. Use of topical anti-inflammatory cream. Taping of the foot during exercise. Stretching, only if recommended by the physiotherapist.
Recovery
Severs disease is a self limiting condition that gradually resolves as the patient moves towards skeletal maturity. This usually takes between 6 to 12 months, but may persist for as long as 2 years. With appropriate management, symptoms may resolve in a number of weeks. Patients with Severs disease typically improve gradually over time and full function is restored.
Fallen Arch Pain Relief
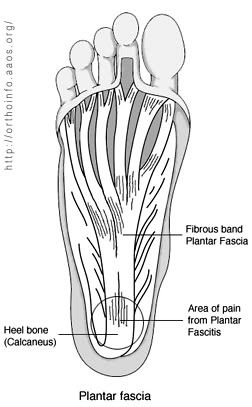
Arch pain is felt on the underside of your foot between the heel and ball. The purpose of the arch is to transfer your body weight from heel to toe, and pain is the result when the arch doesn?t function properly. Your foot actually contains two arches: the longitudinal arch which runs the length of your foot, and the transverse arch (also known as the metatarsal arch) which spans the width of your foot. There are 24 bones which create the arches and these bones are held together through their unique interlocking shapes and ligaments. The muscles and the plantar fascia (a broad band of fibrous tissue which runs from the heel to the toes) provide secondary support, and fat pads help to absorb impact and bear your weight. If any of these structures or their interaction are damaged or faulty, arch pain may occur. The most common cause of arch pain is plantar fasciitis, an inflammation of the plantar fascia. You may also suffer arch pain if you have a structural imbalance in your foot or suffer from arthritis. But arch pain may also result from stepping on a rock or when someone steps on your foot. This force may cause an injury such as a bone fracture or damage to the supporting muscles, ligaments, or tendons underneath your foot.
Causes
Spending a lot of time on your feet. Especially when you are not used to doing so. For example you may have started a new job such as waiting tables where you are on your feet all day and wake up the next day with sore feet. This is a sign of damage and over time could lead to plantar fasciitis. Being Over-Weight. Never an easy topic to discuss but in simple terms, the heavier you are, the greater the burden on your feet. There are times when you're walking when your entire body weight is borne on one leg and therefore one foot, placing great strain on the plantar fascia. Wearing shoes with poor arch support or cushioning. A tight Achilles tendon. This is the big tendon at the bottom of your calf muscles above your heel. If this is excessively tight this can affect your ability to flex your ankle and make you more likely to damage your plantar fascia. Suddenly changing your exercise routine. Using running as an example if you suddenly run many more miles than your are used to or change to a new running surface e.g. grass to tarmac - these factors can put excessive strain on the plantar fascia and lead to plantar fasciitis. All of these risk factors ultimately lead to a specific change in foot structure. The term given is over-pronation and this basically describes rolling in of the foot and lowering of the arches. It is this change that excessively elongates the plantar fascia which can lead to plantar fasciitis.
Symptoms
Common symptoms of plantar fasciitis include pain in the morning when you first get out of bed, pain and stiffness when you start to walk after sitting for a while, increasing arch or heel pain toward the end of the day, tired feet at the end of the day. Other causes of arch and heel pain include arthritis, infection, fractures and sprains, and even certain systemic diseases. Since there are multiple possible causes, you should see your podiatrist for a thorough evaluation if you are experiencing arch or heel pain that does not respond quickly to early treatment.
Diagnosis
A patient is asked to step with full body weight on the symptomatic foot, keeping the unaffected foot off the ground. The patient is then instructed to "raise up on the tip toes" of the affected foot. If the posterior tibial tendon has been attenuated or ruptured, the patient will be unable to lift the heel off the floor and rise onto the toes. In less severe cases, the patient will be able to rise on the toes, but the heel will not be noted to invert as it normally does when we rise onto the toes. X-rays can be helpful but are not diagnostic of the adult acquired flatfoot. Both feet, the symptomatic and asymptomatic - will demonstrate a flatfoot deformity on x-ray. Careful observation may show a greater severity of deformity on the affected side.
Non Surgical Treatment
Rest is the most important thing you can do. Stay off your feet, or use a cane. Gently apply ice to the arch for at least 30 minutes, and repeat every 3 or 4 hours. Apply mild compression to the foot. Use a Fabriform PSC Foot and Ankle Strap to help support the arch, reduce swelling, and relieve pain and fatigue. This strap is easy to apply and adjust for a custom fit. Low profile allows it to fit in any shoe. Allows you to apply just the right amount of arch support/compression for your foot. Before stepping down after sleeping or resting, stretch the arch of your foot by pulling up on the ball of the foot and toes, as far as you comfortably can; hold the foot in this position for ten seconds. Repeat at least ten times. Consideration should also be given to the use of night splints. These are very effective for stretching the plantar fascia to relieve first weight bearing pain.

Surgical Treatment
If you have pain that has not been responsive to other treatments, there is a new non-surgical treatment that was recently approved by the FDA. ESWT (extracorporeal shockwave therapy) uses strong electrohydraulic acoustic (sound) energy that triggers the body?s natural repair mechanism. This treatment method is safe, effective and requires a very short recovery period compared to older surgical techniques.
Prevention
It is possible to prevent arch pain by wearing well-fitting shoes while performing any physical activity. Many times doctors will suggest a therapeutic shoe with a higher heel to relieve the pressure on the achilles tendon and also the arch muscle (plantar fasciitis). People with arch pain suffer from regular flare-ups of pain. However there is no risk to others as this is not a contagious condition.
Stretching Exercises
Flexibility is important in preventing injuries. With a simple stretching exercise, you can rehabilitate the muscles of your foot to relieve arch pain and prevent future injuries. This simple exercise by Tammy White and Phyllis Clapis for Relay Health is a good way to strengthen your foot muscles and stretch your plantar fascia. Sit in a chair and cross one foot over your other knee. Grab the base of your toes and pull them back toward your leg until you feel a comfortable stretch. Hold 15 seconds and repeat three times. When you can stand comfortably on your injured foot, you can begin standing to stretch the plantar fascia at the bottom of your foot.
Flexible Flat Foot In Adults
Overview
Posterior tibial tendon insufficiency (also called posterior tibial tendon dysfunction or adult acquired flatfoot) has been named literally after failure of the posterior tibial tendon. However, the condition is caused not only by the progressive failure of the posterior tibial tendon; it is also failure of associated ligaments and joints on the inner side of the ankle and foot. This results in collapse of the arch of the foot, along with the deformity which most often becomes the debilitating problem in its later stages. While at the beginning the common symptom is pain over the tendon in the inner part of the hindfoot and midfoot, later on it is the deformity that can threaten a person?s ability to walk. Just as the tendon degenerates and loses its function, other soft tissue on the same inner side of the foot - namely the ligaments - degenerate and fail. Ligaments are responsible for holding bones in place, and when they fail, bones shift to places where they shouldn?t; deformity is the result. The deformity causes malalignment, leading to more stress and failure of the ligaments. 
Causes
As discussed above, many health conditions can create a painful flatfoot. Damage to the posterior tibial tendon is the most common cause of AAFD. The posterior tibial tendon is one of the most important tendons of the leg. It starts at a muscle in the calf, travels down the inside of the lower leg and attaches to the bones on the inside of the foot. The main function of this tendon is to hold up the arch and support your foot when you walk. If the tendon becomes inflamed or torn, the arch will slowly collapse. Women and people over 40 are more likely to develop problems with the posterior tibial tendon. Other risk factors include obesity, diabetes, and hypertension. Having flat feet since childhood increases the risk of developing a tear in the posterior tibial tendon. In addition, people who are involved in high impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use. Inflammatory arthritis, such as rheumatoid arthritis, can cause a painful flatfoot. This type of arthritis attacks not only the cartilage in the joints, but also the ligaments that support the foot. Inflammatory arthritis not only causes pain, but also causes the foot to change shape and become flat. The arthritis can affect the back of the foot or the middle of foot, both of which can result in a fallen arch.
Symptoms
Not everyone with adult flatfoot has problems with pain. Those who do usually experience it around the ankle or in the heel. The pain is usually worse with activity, like walking or standing for extended periods. Sometimes, if the condition develops from arthritis in the foot, bony spurs along the top and side of the foot develop and make wearing shoes more painful. Diabetic patients need to watch for swelling or large lumps in the feet, as they may not notice any pain. They are also at higher risk for developing significant deformities from their flatfoot.
Diagnosis
The diagnosis of posterior tibial tendon dysfunction and AAFD is usually made from a combination of symptoms, physical exam and x-ray imaging. The location of pain, shape of the foot, flexibility of the hindfoot joints and gait all may help your physician make the diagnosis and also assess how advanced the problem is.
Non surgical Treatment
What are the treatment options? In early stages an orthotic that caters for a medially deviated subtalar joint ac-cess. Examples of these are the RX skive, Medafeet MOSI device. Customised de-vices with a Kirby skive or MOSI adaptation will provide greater control than a prefabricated device. If the condition develops further a UCBL orthotic or an AFO (ankle foot orthotic) could be necessary for greater control. Various different forms of surgery are available depending upon the root cause of the issue and severity. 
Surgical Treatment
For patients with a more severe deformity, or significant symptoms that do not respond to conservative treatment, surgery may be necessary. There are several procedures available depending on the nature of your condition. Ligament and muscle lengthening, removal of inflamed tendon lining, transferring of a nearby tendon to re-establish an arch, and bone realignment and fusion are examples of surgical options to help with a painful flatfoot condition. Surgery can be avoided when symptoms are addressed early. If you are feeling ankle pain or notice any warmth, redness or swelling in your foot, contact us immediately. We can create a tailored treatment plan to resolve your symptoms and prevent future problems.
Achilles Tendon Repair Cast Iron
Overview  The Achilles tendon is the soft tissue located in the heel which connects calf muscle to the heel bone allowing the body to perform certain activities such as rising on the tip toes and pushing off when running or walking. Achilles tendon tears occur when the tendon becomes torn through excessive pressure put on the area which the tendon is unable to withstand. Tears are most commonly found when suddenly accelerating from a standing position and therefore is often seen in runners and athletes involved in racquet sports. A tear can also occur when a continuous force is being put on the heel through prolonged levels of activity and overuse however this can also occur as a result of sudden impact or force to the area common in contact sports such as rugby and hockey. Although Achilles tendon tears can range in their severity, a rupture is the most serious form of tear and involves a completely torn tendon. This injury is more common in patients in their 30?s and 40?s. Causes The tendon usually ruptures without any warning. It is most common in men between the ages of 40-50, who play sports intermittently, such as badminton and squash. There was probably some degeneration in the tendon before the rupture which may or may not have been causing symptoms. Symptoms Tendon strain or tendon inflammation (tendonitis) can occur from tendon injury or overuse and can lead to a rupture. Call your doctor if you have signs of minor tendon problems. Minor tenderness and possible swelling increases with activity. There is usually no specific event causing sudden pain and no obvious gap in the tendon. You can still walk or stand on your toes. Acute calf pain and swelling can indicate a tear or partial tear of the Achilles tendon where it meets the calf muscle. You may still be able to use that foot to walk, but you will need to see a specialist such as an orthopedic surgeon. Surgery is not usually done for partial tears. Sometimes special heel pads or orthotics in your shoes may help. Follow up with your doctor to check for tendonitis or strain before resuming activity, because both can increase the risk of tendon rupture. Any acute injury causing pain, swelling, and difficulty with weight-bearing activities such as standing and walking may indicate you have a tear in your Achilles tendon. Seek prompt medical attention from your doctor or emergency department. Do not delay! Early treatment results in better outcome. If you have any question or uncertainty, get it checked. Diagnosis A detailed history, and examination by an appropriately qualified health professional, will allow a diagnosis to be made. An ultrasound or MRI scan can confirm the diagnosis. Other causes of symptoms in the area, such as those referred from the lumbar spine and local infection, should be excluded. Non Surgical Treatment Your doctor may advise you to rest your leg and keep the tendon immobile in a plaster cast while it heals. Or you may need to have an operation to treat an Achilles tendon rupture. The treatment you have will depend on your individual circumstances, such as your age, general health and how active you are. It will also depend on whether you have partially or completely torn your tendon. If you have a partial tear, it might get better without any treatment. Ask your doctor for advice on the best treatment for you. If you need pain relief, you can take over-the-counter painkillers such as paracetamol or ibuprofen. Always read the patient information that comes with your medicine and if you have any questions, ask your pharmacist for advice.
The Achilles tendon is the soft tissue located in the heel which connects calf muscle to the heel bone allowing the body to perform certain activities such as rising on the tip toes and pushing off when running or walking. Achilles tendon tears occur when the tendon becomes torn through excessive pressure put on the area which the tendon is unable to withstand. Tears are most commonly found when suddenly accelerating from a standing position and therefore is often seen in runners and athletes involved in racquet sports. A tear can also occur when a continuous force is being put on the heel through prolonged levels of activity and overuse however this can also occur as a result of sudden impact or force to the area common in contact sports such as rugby and hockey. Although Achilles tendon tears can range in their severity, a rupture is the most serious form of tear and involves a completely torn tendon. This injury is more common in patients in their 30?s and 40?s. Causes The tendon usually ruptures without any warning. It is most common in men between the ages of 40-50, who play sports intermittently, such as badminton and squash. There was probably some degeneration in the tendon before the rupture which may or may not have been causing symptoms. Symptoms Tendon strain or tendon inflammation (tendonitis) can occur from tendon injury or overuse and can lead to a rupture. Call your doctor if you have signs of minor tendon problems. Minor tenderness and possible swelling increases with activity. There is usually no specific event causing sudden pain and no obvious gap in the tendon. You can still walk or stand on your toes. Acute calf pain and swelling can indicate a tear or partial tear of the Achilles tendon where it meets the calf muscle. You may still be able to use that foot to walk, but you will need to see a specialist such as an orthopedic surgeon. Surgery is not usually done for partial tears. Sometimes special heel pads or orthotics in your shoes may help. Follow up with your doctor to check for tendonitis or strain before resuming activity, because both can increase the risk of tendon rupture. Any acute injury causing pain, swelling, and difficulty with weight-bearing activities such as standing and walking may indicate you have a tear in your Achilles tendon. Seek prompt medical attention from your doctor or emergency department. Do not delay! Early treatment results in better outcome. If you have any question or uncertainty, get it checked. Diagnosis A detailed history, and examination by an appropriately qualified health professional, will allow a diagnosis to be made. An ultrasound or MRI scan can confirm the diagnosis. Other causes of symptoms in the area, such as those referred from the lumbar spine and local infection, should be excluded. Non Surgical Treatment Your doctor may advise you to rest your leg and keep the tendon immobile in a plaster cast while it heals. Or you may need to have an operation to treat an Achilles tendon rupture. The treatment you have will depend on your individual circumstances, such as your age, general health and how active you are. It will also depend on whether you have partially or completely torn your tendon. If you have a partial tear, it might get better without any treatment. Ask your doctor for advice on the best treatment for you. If you need pain relief, you can take over-the-counter painkillers such as paracetamol or ibuprofen. Always read the patient information that comes with your medicine and if you have any questions, ask your pharmacist for advice.  Surgical Treatment Unlike other diseases of the Achilles tendon such as tendonitis or bursitis, Achilles tendon rupture is usually treated with surgical repair. The surgery consists of making a small incision in the back part of the leg, and using sutures to re-attach the two ends of the ruptured tendon. Depending on the condition of the ends of the ruptured tendon and the amount of separation, the surgeon may use other tendons to reinforce the repair. After the surgery, the leg will be immobilized for 6-8 weeks in a walking boot, cast, brace, or splint. Following this time period, patients work with a physical therapist to gradually regain their range of motion and strength. Return to full activity can take quite a long time, usually between 6 months and 1 year.
Surgical Treatment Unlike other diseases of the Achilles tendon such as tendonitis or bursitis, Achilles tendon rupture is usually treated with surgical repair. The surgery consists of making a small incision in the back part of the leg, and using sutures to re-attach the two ends of the ruptured tendon. Depending on the condition of the ends of the ruptured tendon and the amount of separation, the surgeon may use other tendons to reinforce the repair. After the surgery, the leg will be immobilized for 6-8 weeks in a walking boot, cast, brace, or splint. Following this time period, patients work with a physical therapist to gradually regain their range of motion and strength. Return to full activity can take quite a long time, usually between 6 months and 1 year.
Are Fallen Arches Flat Feet?
_(B)_Adult_foot_that_has_never_worn_shoes,_(Right)_(A)_Foot_of_a_boy_who_has_worn_shoes_for_just_a_few_weeks._Plaster_casts.jpg)
A variety of foot problems can lead to adult acquired flatfoot deformity (AAFD), a condition that results in a fallen arch with the foot pointed outward. Most people - no matter what the cause of their flatfoot - can be helped with orthotics and braces. In patients who have tried orthotics and braces without any relief, surgery can be a very effective way to help with the pain and deformity. This article provides a brief overview of the problems that can result in AAFD. Further details regarding the most common conditions that cause an acquired flatfoot and their treatment options are provided in separate articles. Links to those articles are provided.
Causes
Most cases of flatfeet are simply the result of normal development. When that is not the case, the condition can be caused by a number of factors, including the following, Age, disease, injury, obesity or being overweight, physical abnormality, pregnancy. Flattened arches in adults may result from the stresses of aging, weight gain, and the temporary increase in elastin (protein in connective tissue) due to pregnancy. In some cases, flatfeet are caused by a physical abnormality, such as tarsal coalition (two or more bones in the foot that have grown together) or accessory navicular (an extra bone along the side of the foot). The effects of diseases such as diabetes and rheumatoid arthritis can lead to flatfeet. An injury (e.g., bone fracture, dislocation, sprain or tear in any of the tendons and ligaments in the foot and leg) also can cause flatfeet.
Symptoms
Having flat feet can be painless and is actually normal in some people. But others with flat feet experience pain in the heel or arch area, difficulty standing on tiptoe, or have swelling along the inside of the ankle. They may also experience pain after standing for long periods of time or playing sports. Some back problems can also be attributed to flat feet.
Diagnosis
You can test yourself to see if you have flat feet or fallen arches by using a simple home experiment. First, dip your feet in water. Then step on a hard flat surface, like a dry floor or a piece of paper on the floor, where your footprints will show. Step away and examine your foot prints. If you see complete/full imprints of your feet on the floor, you may have fallen arches. However, it?s important to seek a second option from a podiatrist if you suspect you have fallen arches so they can properly diagnose and treat you.
Non Surgical Treatment
The treatment your podiatrist recommends will depend upon the trouble and pain you?re experiencing. Custom shoe inserts (orthotics) are most often recommended and are quite effective. Stretching exercises to loosen and strengthen the supporting tendons may also be recommended. Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may recommend an ankle brace or a custom orthotic device that fits into your shoe to support the arch. A short-leg cast or boot may be worn to immobilize the foot and allow the tendon to heal. Ultrasound therapy and stretching exercises may help rehabilitate the tendon and muscle following immobilization. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Your foot and ankle surgeon may recommend changes in your footwear.
Surgical Treatment

Generally one of the following procedures is used to surgically repair a flat foot or fallen arch. Arthrodesis. One or more of your bones in the foot or ankle are fused together. Osteotomy. Correcting alignment by cutting and reshaping a bone. Excision. Removing a bone or a bone spur. Synovectomy. Cleaning the sheath that covers the tendon. Tendon transfer. Using a piece of one tendon to lengthen or replace another. Arthroereisis. placing a small device in the subtalar joint to limit motion. For most people, treatment is successful, regardless of the cause, although the cause does does play a major role in determining your prognosis. Some causes do not need treatment, while others require a surgical fix.
Prevention
oll away pain. If you're feeling pain in the arch area, you can get some relief by massaging the bottom of your foot. A regular massage while you're watching TV can do wonders" Stretch out. Doing the same type of stretching exercises that runners do in their warm-up can help reduce arch pain caused by a tight heel cord. One of the best exercises is to stand about three feet from a wall and place your hands on the wall. Leaning toward the wall, bring one foot forward and bend the knee so that the calf muscles of the other leg stretch. Then switch legs. Stretching is particularly important for women who spend all week in heels and then wear exercise shoes or sneakers on weekends. Get measured each time you buy new shoes. Don't assume that since you always wore a particular size, you always will. Too many people try to squeeze into their 'regular' shoe size and wind up with serious foot problems or sores on their feet. When your arch is falling, your feet may get longer or wider and you may or may not feel pain, so getting your foot measured each time you buy shoes is a good indicator of your arch's degeneration. Examine your shoes. If the heel is worn down, replace it. But if the back portion of the shoe is distorted or bent to one side, get yourself into a new pair of supportive shoes like those made specifically for walking. That's because flat feet can affect your walking stride, and failing to replace worn shoes may lead to knee or hip pain.
Fallen Arches What To Expect

Flat feet plague many Americans and perhaps one of the worst times to have fallen arches is the winter holiday season. Why? Many people are destined to spend hours standing in line waiting to pay for holiday gifts, see Santa or mail holiday cards and packages. There are also those cocktail parties, holiday caroling sessions and strolls through the Christmas lights that will undoubtedly have people on their feet for long stretches of time too.
Causes
Flat feet in adults can arise from a variety of causes. Here are the most common. An abnormality that is present from birth, stretched or torn tendons, damage or inflammation of the posterior tibial tendon (PTT), which connects from your lower leg, along your ankle, to the middle of the arch, broken or dislocated bones. Some health conditions, such as rheumatoid arthritis, Nerve problems. Other factors that can increase your risk include obesity, diabetes, ageing and Pregnancy.
Symptoms
Many people have flat feet and notice no problems and require no treatment. But others may experience the following symptoms, Feet tire easily, painful or achy feet, especially in the areas of the arches and heels, the inside bottom of your feet become swollen, foot movement, such as standing on your toes, is difficult, back and leg pain, If you notice any of these symptoms, it's time for a trip to the doctor.
Diagnosis
If your child has flatfeet, his or her doctor will ask about any family history of flatfeet or inherited foot problems. In a person of any age, the doctor will ask about occupational and recreational activities, previous foot trauma or foot surgery and the type of shoes worn. The doctor will examine your shoes to check for signs of excessive wear. Worn shoes often provide valuable clues to gait problems and poor bone alignment. The doctor will ask you to walk barefoot to evaluate the arches of the feet, to check for out-toeing and to look for other signs of poor foot mechanics. The doctor will examine your feet for foot flexibility and range of motion and feel for any tenderness or bony abnormalities. Depending on the results of this physical examination, foot X-rays may be recommended. X-rays are always performed in a young child with rigid flatfeet and in an adult with acquired flatfeet due to trauma.
Non Surgical Treatment
Flat feet and fallen arches can be treated effectively by wearing an orthotic insert in your shoes. Orthotics can be custom-made and prescribed by your foot specialist (podiatrist), or you can use a so called pre-made foot orthotic. Most people do not require expensive custom-made orthotics to combat excess pronation, unless they have a specific medical foot condition. Orthotic insoles were developed to correct excess pronation, thereby providing sustainable, long-lasting pain relief to many aches and pains in a natural way. Comfort, Casual and Sports are products which promote excellent biomechanical control of the foot.
Surgical Treatment

A better approach is to strengthen the weakened ligaments with Prolotherapy, supplemented by an arch support if the condition has existed for several years. Chronic pain is most commonly due to tendon and ligament weakness, or cartilage deterioration. The safest and most effective natural medicine treatment for repairing tendon, ligament and cartilage damage is Prolotherapy. In simple terms, Prolotherapy stimulates the body to repair painful areas. It does so by inducing a mild inflammatory reaction in the weakened ligaments and cartilage. Since the body heals by inflammation, Prolotherapy stimulates healing. Prolotherapy offers the most curative results in treating chronic pain. It effectively eliminates pain because it attacks the source: the fibro-osseous junction, an area rich in sensory nerves. What?s more, the tissue strengthening and pain relief stimulated by Prolotherapy is permanent.
Prevention
Wear Supportive Footwear. Spend the money it takes to get proper fitting and quality footwear with good arch supports. Most sufferers of fallen arches and plantar fasciitis are born with high arches that sag as they get older. Good footwear can prevent this from becoming a problem. Flat feet, however, can become just as problematic. So, really we should all be wearing good footwear to avoid this potentially painful condition. Take It Easy. If your heel starts to hurt, take a rest. If the pain doesn?t go away after several days of resting, it may be time to see a podiatrist. Orthotics. Special insoles to support the arch of the foot can provide some much needed help. You can buy these at your local drugstore (not recommended), or you can have them specially made and custom fit for your feet. It can take awhile to get just the right one for your foot, but sometimes it can be just what you needed. Weight Control. Yes, maintaining a sensible diet with your ideal weight can be beneficial in many ways. It makes sense to think that the more weight your arches are supporting, the more easily they will fall and become painful.
Achilles Tendon Pain In The Heel
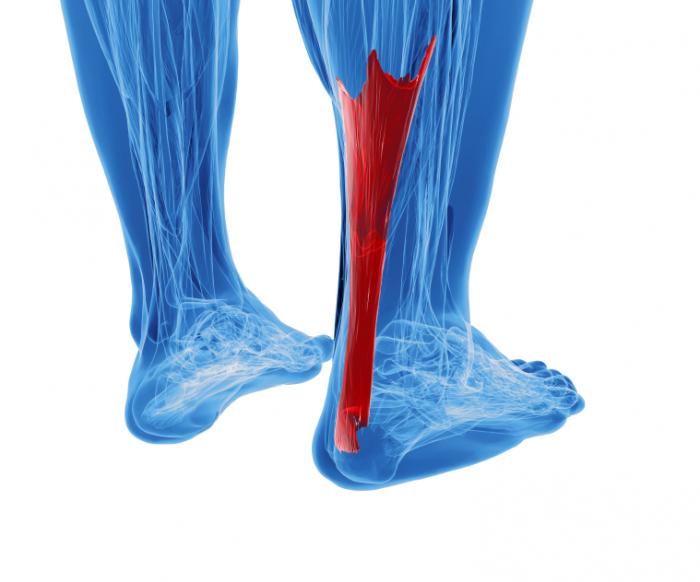 The Achilles tendon connects the calf muscles in the lower leg to the heel bone. It is the largest yet most exposed tendon in the body. Achilles tendonitis is where the Achilles tendon, and sometimes the protective sheath through which it moves, becomes inflamed, causing pain and swelling symptoms. Achilles tendonitis (also known as Achilles tendinopathy or tendonosis) is classified as an overuse injury. If left untreated it can become chronic (long-term), requiring more intensive treatment. Achilles tendonitis can also increase the risk of sustaining an Achilles tendon rupture (tear).
The Achilles tendon connects the calf muscles in the lower leg to the heel bone. It is the largest yet most exposed tendon in the body. Achilles tendonitis is where the Achilles tendon, and sometimes the protective sheath through which it moves, becomes inflamed, causing pain and swelling symptoms. Achilles tendonitis (also known as Achilles tendinopathy or tendonosis) is classified as an overuse injury. If left untreated it can become chronic (long-term), requiring more intensive treatment. Achilles tendonitis can also increase the risk of sustaining an Achilles tendon rupture (tear).
Causes
Short of a trauma, the primary cause of Achilles tendonitis is when the calf muscle is so tight that the heel is unable to come down to the ground placing extreme stress on the Achilles tendon at the insertion. Keep in mind that the calf muscle is designed to contract up, lifting the heel bone off the ground, propelling you forwards to the front of the foot for push off. When the calf is so tight that the heel is prevented from coming down on the ground there will be stress on the tendon and the foot will over pronate causing the Achilles tendon to twist, adding to the stress on the insertion. Improper treatment may lead to a more severe injury, such as a rupture or chronic weakening, which may require surgery.
Symptoms
Symptoms vary because you can injure various areas of the muscle-tendon complex. The pain may be an acute or chronic sharp, stabbing, piercing, shooting, burning or aching. It is often most noticeable immediately after getting out of bed in the morning, or after periods of inactivity, like sitting down for lunch. After a couple minutes of walking around, it will often then settle down somewhat, before becoming symptomatic again after excessive time standing or walking. But regardless of how the pain is perceived, Achilles tendon pain should not be left untreated due to the danger that the tendon can become weak, frayed, thickened, and eventually it may rupture.
Diagnosis
A doctor or professional therapist will confirm a diagnosis, identify and correct possible causes, apply treatment and prescribe eccentric rehabilitation exercises. An MRI or Ultrasound scan can determine the extent of the injury and indicate a precise diagnosis. Gait analysis along with a physical assessment will identify any possible biomechanical factors such as over pronation which may have contributed to the achilles tendonitis and training methods will be considered. Biomechanical problems can be corrected with the use of orthotic inserts and selection of correct footwear.
Nonsurgical Treatment
Massage therapy improves blood flow to the muscles and tissues of the affected area while increasing range of motion and can prevent recurring injury. The healing process can be quickened using ultrasound heat therapy to improve blood flow to the affected area. Wearing a night brace keeps the leg flexed, preventing stiffening of the tendon, which would impair healing. Stretching exercises increase flexibility and allow the tendon to heal without shortening, a deformity resulting in chronic pain. Persistent Achilles pain may warrant the use of a cast or walking boot to be worn for 4-6 weeks stabilizing the tendon so it can heal. After removal of the cast or boot, physical therapy will be ordered to increase functionality of the affected limb. To reduce chronic inflammation of the tendon, corticosteroid injections may be prescribed. It?s important to note that this corticosteroid treatment increases the risk of tendon rupture. Ultrasound imaging may be used by the physician administering the steroid injection, in order to help visualize the affected area. When all other therapies have failed to or tendon rupture occurs, surgical intervention and repair of the muscles and tendons is the last treatment option.

Surgical Treatment
If non-surgical approaches fail to restore the tendon to its normal condition, surgery may be necessary. The foot and ankle surgeon will select the best procedure to repair the tendon, based upon the extent of the injury, the patient?s age and activity level, and other factors.
Prevention
As with all injuries, prevention is your best defense especially with injuries that are as painful and inconvenient as Achilles tendonitis. Options for how to prevent Achilles tendonitis include, stretching- Stretching properly, starting slowly, and increasing gradually will be critical if you want to avoid Achilles tendonitis. To help maintain flexibility in the ankle joint, begin each day with a series of stretches and be certain to stretch prior to, and after, any exercise or excessive physical activity. Orthotics and Heel Support- Bio-mechanically engineered inserts and heel cups can be placed in your shoes to correct misalignments or bolster the support of your foot and are available without a prescription. The temporary heel padding that these provide reduces the length that the Achilles tendon stretches each time you step, making it more comfortable to go about your daily routine. Proper Footwear- Low-heeled shoes with good arch support and shock absorption are best for the health of your foot. Look into heel wedges and other shoe inserts to make sure that your everyday foot mechanics are operating under ideal conditions.